Ophthalmic
viscosurgical devices (OVDs) are being used successfully in many ophthalmic
surgeries, most commonly in cataract surgery1. OVDs help in cataract
surgery by maintaining the depth and shape of anterior chamber (AC) especially
in the stages of capsulorhexis and IOL implantation2. They also
provide viscous protection to the delicate corneal endothelium from surgically
induced trauma3.
Based
on their rheological properties OVDs have been classified as cohesive and
dispersive4. The cohesive OVDs have high viscosity, high molecular
weight and contain long molecular chains, dispersive OVDs like
hydroxypropylmethylcellulose 2% (HPMC) have lower viscosity with shorter
molecular chains that have less tendency to entangle5.
Use of
OVDs in cataract surgery can be associated with adverse effects; the most commonly
and potentially dangerous is the rise, usually transient, in post-operative
intra ocular pressure (IOP)6. To prevent this complication, the OVD
should be removed through aspiration after intraocular lens (IOL) implantation;
however, an OVD located in the ciliary sulcus or behind the IOL may not be
easily removed.
Hydro-implantation
is a technique of implanting IOL under continuous irrigation from either
irrigation cannula of phacoemulsification machine or Simco cannula without
using OVDs.
We conducted a study to
evaluate the effect on IOP following phacoemulsification with
IOL implantation by either using OVD (HPMC 2%) or hydro-implantation of
IOL.
MATERIAL AND METHODS
This comparative, prospective study with
convenience (Non Probability) sampling was conducted from September 2011 to
March 2012 at LRBT Eye Hospital Mandra, Rawalpindi. Patients with ages from 50
years to 75 years were selected for the study. The patients were first allotted
the hospital registration number before proceeding to the examination. Complete
eye examination was performed. Eyes with senile uncomplicated
cataracts were selected.
Patients
with pre-operatively raised IOP, previous history of glaucoma or narrow/closed
angle on gonioscopy were excluded. Dark brown cataracts were also excluded
because of a likelihood of converting to ECCE or prolonged phacoemulsification time. Cases that had any serious
complication like posterior capsule rent with or without vitreous loss were
also excluded from the study. One hundred patients meeting the inclusion and
exclusion criteria were selected for the study and were divided into two
groups, A and B of 50 patients each. The study procedure and its aims were explained to all
the patients before beginning the treatment and
they had to sign on informed written consent form.
Pre-operative
IOP (baseline IOP) was again checked and recorded one day prior to surgery.
A
3.25mm clear corneal incision and two side ports were constructed at 10 and 2 O’clock
positions in all patients. Anterior chamber (AC) was filled with HPMC and
capsulorhexis was carried out. Phacoemulsification was done with same technique
in both groups.
In
group A after completion of phacoemulsi-fication, incision was enlarged to
5.5mm after maintenance of AC and capsular bag with HPMC and 5.5mm rigid PMMA
IOL was secured in capsular bag. HPMC was aspirated thoroughly from the AC, the
angle, the capsule fornix and the retrolenticular space using Simco cannula.
Side ports and main incision were sealed with stromal hydration.
In
group B after completion of phacoemulsi-fication, incision was enlarged after
maintaining the AC by the inflow of the fluid from the Simco cannula held in
non dominant side’s side port (left side in our case). PMMA IOL was held with
McPherson forceps in the right hand and advancing haptic of IOL was inserted
through the main incision, pushing it forward and downward, with an angle of
45-50 degrees, securing it in the capsular bag. Through main incision, with the
IOL dialer, IOL was engaged from the haptic-optic junction. With a forward,
downward and clockwise movement trailing haptic was secured in the capsular
bag. As no OVD was used for implantation of IOL, no removal of OVD was
required. Side ports and main incision were sealed with stromal hydration.
IOP measurements were done at 24 hours and 1 week post-operatively
in both groups and were compared with the baseline IOP (preoperative). IOP
measurement was carried out by the same ophthalmologist on same instrument used
for pre-operative IOP measurement.
Analysis of the data was
carried out using statistical package for social sciences (SPSS) version 13.0.
Student ‘t’ test was used to compare the mean IOP of each group at each time
interval. ‘t’ test was also applied for comparison of results between the two
groups. A p-value < 0.05 was used as significance cut off point.
RESULTS
Data of
100 patients (47 males and 53 females) was analyzed. Out of those, 50 (24 males
and 26 females) were in group A (2% HPMC group) and 50 (23 males and 27
females) were in group B (hydro-implantation group). Age spectrum was from 56
to 72 years in group A and from 54 to 74 years in group B. The age difference
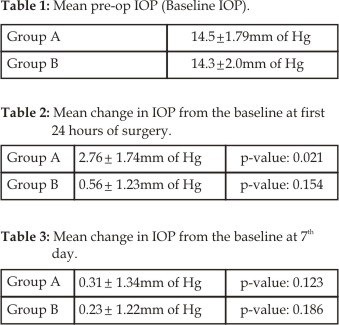
between the two groups was statistically insignificant (p-value: 0.275). There
was no significant difference in mean pre-operative IOP of both groups (p-value:
0.483), Table 1. No patient in either group had a pre-operative IOP greater
than 19mm of Hg. Group A experienced statistically significant elevation in
mean IOP at first 24 hours after surgery, over the pre-operative values (p-value: 0.021),
Table-2. Elevation in mean IOP in Group B at first 24 hours after surgery was
found insignificant over the pre-operative values (p-value: 0.154), Table-2. Difference
between mean post-operative IOP of the two groups at 24 hours after surgery was
also compared and found significant (p-value: 0.032). On 7th day
after surgery, mean change in IOP from their respective baselines in both
groups was found insignificant and IOP in both groups had returned
approximately to the pre-operative values, Table 3.
Moreover, the mean IOP values
at 7th post-operative day were also comparable between the two
groups (p-value: 0.420).
DISCUSSION
Elevated
IOP is common post-operative complication following phacoemulisification7.
OVD remaining in the eye may cause mechanical obstruction of the trabecular
meshwork and is a major cause for early post-operative rise in IOP8.
The particles of low-viscosity
OVDs like HPMC are considered dispersive, because they do not adhere to one
another. Dispersive OVDs protect individual structures in the anterior chamber
such as the corneal endothelium better than cohesive OVD9. However,
low-viscosity OVDs are generally more difficult to remove from the eye
completely because of their dispersive nature10.
Arshinoff had published multiple
studies comparing different OVDs4,11-13. He concluded that, if not
completely removed, all OVDs cause post-operative increases in IOP. According
to Arshin off et al, all high-viscosity OVDs are associated with higher post-operative
IOPs (although not necessarily above 21mm Hg) compared with lower-viscosity
OVDs. He concluded that retained viscoelastic and predispose-tions like
trabecular insult or undiagnosed glaucoma are the main causes of post-operative
rises in IOP.
A local study conducted by
Waseem et al14 compared the effect on IOP between HPMC and sodium
hyaluronate (Cohesive OVD) and concluded that IOP rises in both groups but more
significantly in sodium hyaluronate group.
In 1983, Berson et al15
also reported that sodium hyaluronate when injected into the anterior chamber
caused increase in IOP ranging from 55 to 60mm of Hg due to blockade of
trabecular meshwork.
Thorough removal of OVD is
vital for avoidance of a post-operative IOP increase. However, complete removal
of the OVD behind the IOL is known to be difficult. Several surgical techniques
for removal of OVD, particularly from behind the IOL, have been described16,
however, complete avoidance of a post-operative IOP increase has not been
achieved with any technique.
In our study, we used hydro-implantation
technique for IOL implantation in one group. No spike of raised IOP was
recorded at any time interval in this group. This indicates that hydro-implantation
did reduce the risk for elevated post-operative IOP. Our results are augmented
by a study conducted by Tak17 for foldable IOL implantation using
hydro-implantation.
The
learning curve of the technique is short but the beginner might find some
difficulties in implantation IOL with this technique initially. In case of any
difficulty, surgeon can always shift back to conventional method of IOL
implantation with OVD.
CONCLUSION
We conclude that hydro-implantation
technique can reduce the risk for post-operative high IOP and related ocular
co-morbidities.
Author’s Affiliation
Dr. Sohail Zia
Senior Registrar Eye Department
Islamic International Medical
College
Pakistan
Railways Hospital, Rawalpindi
Dr. Yasir Iqbal
Senior Registrar Eye Department
Islamic International Medical
College
Pakistan Railways Hospital, Rawalpindi
Dr. Khalid Masood Ashraf
Layton Rahmatulla Benevolent Trust (LRBT)
Eye Hospital, G. T. Road, Mandra
Rawalpindi
Dr. Aneeq Mirza
Professor and Head of Eye
Department
Islamic International Medical
College
Pakistan Railways Hospital
Rawalpindi
REFERENCES
1.
Larson RS,
Lindstrom RL,
Skelnik DL.
Viscoelastic agents. CLAO J.
1989; 15: 151-60.
2.
Bissen-Miyajima H. Ophthalmic viscosurgical devices. Curr Opin Ophthalmol. 2008;
19: 50–4.
3.
Storr-Paulsen
A, Nørregaard JC, Farik G, Tarnhoj J. The influence of viscoelastic substances
on the corneal endothelial cell population during cataract surgery: a
prospective study of cohesive and dispersive viscoelastics. Acta Ophthalmol Scand. 2007;
85: 183–7.
4.
Arshinoff S. New terminology: ophthalmic viscosurgical
devices. J Cataract Refract
Surg. 2000; 26: 627–8.
5.
Pandey S, Thakur J, Werner L, Izak A,
Apple D. Update on
ophthalmic viscosurgical devices. Agarwal S, Agarwal A, Agarwal A. Phacoemulsification. 3rd ed.
6.
Vajpayee R, Verma K, Sinha R, Titiyal
J, Pandey RM, Sharma N.
Comparative evaluation of efficacy and safety of ophthalmic viscosurgical
devices in phacoemulsification. BMC
Ophthalmol. 2005; 5:
17.
7.
Dooley
I, Beatty S. Discussion of changes in intraocular
pressure and anterior morphometry following phacoemulsification cataract
surgery. Arch Ophthalmol. 2012; 130: 949-50.
8.
Bömer TG, Lagrèze WD, Funk J. Intraocular pressure rise after
phacoemulsification with posterior chamber lens implantation: effect of
prophylactic medication, wound closure, and surgeon's experience. Br J Ophthalmol. 1995;
79: 809-13.
9.
Bollinger K, Smith S. Ophthalmic viscosurgical devices.
10.
Oshika T, Okamoto F, Kaji Y,
Hiraoka T, Kiuchi T, Sato M, Kawana K. Retention
and removal of a new viscous dispersive ophthalmic viscosurgical device during
cataract surgery in animal eyes. Br J Ophthalmol. 2006; 90:
485-7.
11.
Arshinoff SA, Jafari M.
New classification of ophthalmic viscosurgical devices. J Cataract Refract Surg.
2005; 31: 2167-71.
12.
Arshinoff SA, Wong E.
Understanding, retaining and removing dispersive and pseudo dispersive
ophthalmic viscosurgical devices. J Cataract Refract Surg. 2003; 29: 2318-23.
13.
Arshinoff SA, Albiani DA, Taylor-Laporte J.
Intra-ocular pressure after bilateral
cataract surgery using Healon, Healon5, and Healon GV. J Cataract
Refract Surg. 2002; 28: 617-25.
14. Waseem M,
Rustam N,
Qamar ul
Islam. Intraocular pressure after phacoemulsification using hydroxy-propylmethylcellulose and sodium hyaluronate as viscoelastics. J Ayub Med Coll Abbottabad.
2007; 19: 42-5.
15. Berson
FG, Patterson MM, Epstein DL.
Obstruction of aqueous outflow by sodium hyaluronate in enucleated human eyes. Am J Ophthalmol. 1983;
95: 668-72.
16. H Y Lee,
Y J Choy,
J S Park.
Comparison of OVD and BSS for maintaining the Anterior Chamber during IOL
implantation. Korean J
Ophthalmol. 2011;
25: 15-21.