Trauma
to the eye may result in various injuries including presence of blood in the
anterior chamber without perforation of the eye. Closed-globe traumatic
hyphaema may cause diverse complications including associated traumatic uveitis
which generally accompanies the initiating trauma, secondary haemorrhage,
corneal blood staining, synechia formation, and ocular hypertension /
secondary glaucoma.1,2 Aim of management is primarily to prevent
these sight-threatening complications from occurring, or if that fails, treat
them if they arise. Treatment of complications when they arise is fairly
straightforward, but preventing them from occurring is a challenge, arising
from difficulty in predicting who among patients will develop any of these
complications. The result is differences of approach among ophthalmologists and
thus to different management practices. These practices and associated
controversies include advantage of ancillary measures like hospitalization, bed
rest with restriction of activities versus ambulation and at-home treatment;3,4
utility of padding the affected eye or both eyes;5.6 and the place
and usefulness of various medications topical, oral and systemic in preventing
complications.
Numerous studies disclose
conflicting results as to benefit derivable from various medications commonly
used in traumatic hyphaema1,6-8 resulting in many ophthalmologists
in parts of the world either commonly using and recommending them, while others
do not.3,5,6,9,10 Surveys of ophthalmologists in Texas11,
USA disclosed absence of agreement in virtually all aspects of management; and
in the UK,12 divergent views on appropriate medications were
expressed by ophthalmologists. This study is designed to disclose views and
practices of Nigerian ophthalmologists concerning the various medications they
use routinely in uncomplicated closed-globe traumatic hyphaema so as to
determine the dominant views among them in this regard. In the absence of a
multi-center case-control study it is hoped the results obtained from a broad
base of practitioners would act as a guide in the Nigerian and similar
environment.
MATERIAL AND METHODS
A convenience sampling of
Nigerian ophthalmologists who attended the afternoon scientific session on the
16th September 2008 of the annual general congress of the ophthalmological society of Nigeria (OSN) at
Ile Ife in by means of a semi-structured pre-tested questionnaire. Responses
were analyzed with SPSS 11 software.
RESULTS
One
hundred and seven questionnaires were distributed; 101 were retrieved, but 8
were discarded because filling was substantially incomplete, resulting in 93
used for this analysis.
Respondents were from 42 eye
care centers. Of these 93 practitioners, 9 ophthalmologists practice in 4
private eye care facilities and 84 represented 38 public hospitals-tertiary and
secondary. Public eye care centers captured in the study is estimated to
constitute about 75% of such institutions in Nigeria. Among the practitioners,
92.5% declared that resort to surgery was infrequent in traumatic closed globe
hyphaema, and they found non-surgical means usually adequate for preventing and
treating of most complications. Results are presented in tables 1-3, and in Fig.
1.
DISCUSSION
ANCILLARY MANAGEMENT
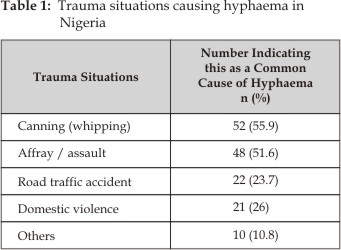
Complications
of traumatic hyphaema as depicted in figure 1 can result in loss of vision, and
treatment is aimed at preventing this complication occurring or reducing their
potential for causing loss of vision. The specific causes of traumatic hyphaema
in Nigeria as depicted in table 1 do not tend to be more amenable to
non-surgical treatment as far as we know.
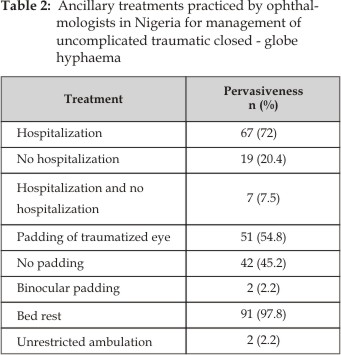
Part of
traditional management of hyphaema patients involved hospital admission and
restriction of activities in the form of bed rest. The patient was required to
lie in bed with the head and shoulder raised to 30 45 degrees and both eyes
were covered with a rigid shield. Medications used included topical
cycloplegics and glucocorticoids, oral sedatives and sometimes prednisone
tablets 2. These measures were thought to be useful in preventing secondary
haemorrhage: activity restriction to reduce stress induced raised venous
pressure, binocular patching to prevent accommodative and pupillary activity
that might induce dislodgement of clot blocking the torn vessel and result in
secondary haemorrhage. It is apparent from table 2 that Nigerian
ophthalmologists in large measure still practice these methods. This is because
of its claimed benefits and the pressure of tradition.
The value of head up position
is to better estimate level of blood and thus classify the hyphaema, determine
if it is decreasing or increasing, facilitate drainage from wider lower
trabecular meshwork, and to have a hyphaema level below pupillary level for
ease of ophthalmoscopy and faster recovery of vision for visual acuity
assessment.13 This appears more of an empirical treatment since the
head-up position is utilized in all grades of hyphaema-those with fluid level
below the pupil, and even in the presence of clots. Unfortunately if the
inferior angle is the part damaged, the head-up position is valueless, and
could in fact be deleterious as the rate of decrease of hyphaema may be
compromised.
Fig. 1: (Okosa and Onyekwe) Complications observed by
Nigerian ophthalmologists on patients with traumatic hyphaema
Although
studies with regards to hospitalization, padding and bed rest were found by
investigators not to influence complication rate, duration of hyphaema and
final visual acuity3,4,5,6 many ophthalmologists in many
institutions still practice and recommend them to varying degrees. These
different approaches are reflected among Nigerian ophthalmologists: 97.8%
insist on bed rest with head-up position, although 72% routinely admit all
patients with closed-globe hyphaema on initial contact.
Reason
for seeming preference for hospitalization is that all patients with hyphaema
require daily examination and monitoring of intra-ocular pressure and other
complications; and it is not possible to monitor for these with patient at
home. Compliance with bed rest and medication in a patient at home cannot be
monitored. Patients may find it inconvenient, or sometimes impossible, to come
from far distances daily, and at the time required for necessary follow-op,
making it seem prudent to admit them.
Padding of affected eye is not
as widespread as bed rest or hospital admission as uniocular patching is
deployed by 54.8%; as against 45.2% who do not pad at all, while 2.5% pad both
eyes. Explanation of the seeming preference for eye padding is to shield the
injured eye and prevent further trauma and secondary haemorrhage although
studies have not demonstrated any differences in complication rate or
requirement for surgery between patients who had eye pad and others who do not5,6.
Topical Medications
Table
3: Drugs routinely used by Nigerian ophthalmo-logists, and their
frequency for management of traumatic non-penetrating hyphaema
|
Glucocorticoid eye drops/ ointment |
81 (87.1) |
|
Atropine and other cycloplegics |
75 (80.6) |
|
Carbonic anhydrase inhibitors (CAI) tablets |
55 (59.1) |
|
Gluco-corticoid eye drops + cycloplegic agent + CAI |
47 (50.5) |
|
Vitamin C tablets 100 mg tid |
10 (10.8) |
|
NSAID eye drops + tablet |
3 (3.2) |
|
Sedatives: diazepam 5 mg bid for adults |
3 (3.2) |
|
Acetaminophen tablets 500mg -1000mg tid for adults |
2 (2.2) |
|
Antibiotic eye drops |
2 (2.2) |
|
Pilocarpine eye drop 1% |
1 (1.1) |
|
NSAID eye drop |
1 (1.1) |
|
Amino-caproic acid |
1 (1.1) |
|
No routine medication |
8 (8.8) |
A preponderant majority (91.4%)
of Nigerian ophthalmologists, as displayed in Table 3, routinely use single or
combination of medications as only 8 of the 93 sampled do not use any
medication in uncomplicated hyphaema. Cycloplegic and glucocor-ticoid eye drops
the most commonly used combination, are deployed with the expectations that by
stabilizing the iris blood vessels, they will control anterior uveitis
resulting from the trauma or presence of blood in the anterior chamber, which
inflammation was both a source of discomfort to the patient, and thought to
predispose to secondary haemorrhage14. Additionally these
medications prevented synaechia formation in hyphaema of long duration; and pupillary
dilatation caused by mydriatics allowed an earlier visual acuity assessment in
clearing hyphaema. The plethora of practices no doubt reflects effect of
diverse and conflicting reports by investigators in this matter. For example
Oksala found topical steroid and cycloplegics reduced re-bleed rate in addition
to treating associated anterior uveitis,14 but a study in Kuwait
City did not find any difference in resolution of traumatic hyphaema, the
complication rate or requirement for surgery among three groups of patients:
those treated with combination of topical cycloplegic agent with
corticosteroid; those treated with corticosteroid eye drops only; and those
treated with placebo in the form of artificial tears.6 It is not
known what factors are responsible for differing effects of these drugs in
these different population groups. Could it be related to diet, habit, blood
group, tissue types, and mechanism of injury? Until these questions are
answered, it appears the practice among Nigerian ophthalmologists is to err on
the side of safety by administering these drugs. It might be argued that
cycloplegics by bunching the iris towards the anterior chamber angle may impede
rate of drainage and raise the IOP, and by its weakening effect on the iris
muscle result in more frequent incidences of re-bleeding; or that miotics would
have the opposite effect. However Rakusin found no difference in complication
rate and resolution of hyphaema among patients treated with miotics,
mydriatics, both or none.7 Conclusion from these studies is that
ancillary and medical treatments have not been conclusively proved to influence
the spontaneous resolution of hyphaema, reduce its complication rate or
decrease need for surgery. This not withstanding routine use of topical
cycloplegic and glucocorticoid drugs in this condition by a vast majority of
Nigerian ophthalmologists is a practice shared by many, but by no means all, of
their contemporaries in other places.1,3,5,8 Reasons for persistence
in use of these medications prophylac-tically include that old practices die
hard especially if they are not demonstrably harmful, and could cause some
good. Besides it is probably more satisfying for the patient and the doctor to
be seen as doing something instead of not treating the patient. Very few
ophthalmologists would be able to send a patient with uncomplicated closed globe
hyphaema home, without padding, no bed rest, and no drug despite reports that
these measures are probably not helpful. Perhaps legal and ethical
consideration in the present situation of uncertain knowledge concerning
possible benefits compel practitioners to offer probably unnecessary treatment in
this condition corresponding to the assertions of Romano and Phillips.10 Why do the few (8.6%) found in current study
not give any medications routinely in uncomplicated hyphaema? The reason is
probably because it would appear as bad science, pointless, and not
evidence-based to subject patients to expenses and inconvenience of treatment
without demonstrable good as the outcome.
Oral Medications
Ophthalmologists
in the UK were unanimous in agreeing on absence of any place for use of
systemic medications in uncomplicated hyphaema12 except for carbonic
anhydrase inhibitors (CAI) which were used by 54% of them for adult patients
with an IOP of above 25 mm Hg. This contrasts with situation among Nigerian
ophthalmologists in which 73% use at least one oral medication routinely (table
3). Carbonic anhydrase inhibitors, is commonest oral medication, and are used
routinely by 59.1% of Nigerian ophthal-mologists as a pro-active measure in all
patients with hyphaema, to prevent secondary glaucoma, especially in large
volume hyphaema. It is not clear why topical pressure lowering agents are not
preferably used rather than oral CAI as some of them are quite affordable,
available and have less adverse reactions.
Use of
NSAIDs however is not popular, being employed by only four ophthalmologists- as
tablets by three (3.2%) and as tablet and topically by one (1.1%). The
rationale for its use appears to be to prevent clot formation and quicken
resolution time of hyphaema. However its efficacy in these has not been demons-trated
in any study, to our knowledge, but rather its use in hyphaema has been
associated with re-bleeding.2 In present survey three of the four
practitioners (75%) who routinely used NSAIDs as oral medication in
uncomplicated hyphaema reported secondary haemorrhage as a frequent
complication, one reported a frequent need for surgical evacuation of hyphaema;
only 36.7% of those who do not use NSAIDs reported re-bleeding as a frequent
complication.
Oral fibrinolytic agents
-amino-caproic acid (ACA) and tranexamic acid are in the main not used,
probably because of lack of availability, cost and perhaps contradictory, and
adverse effects reported by some investigators, and bias of practitioners
against them.2,5,15,10 Topical ACA is currently not available in Nigeria
to the authors knowledge. Use of oral sedatives, acetaminophen tablets and
topical antibiotics are also not as popular as use of oral carbonic anhydras
inhibitors or topical glucocorticoids and atropine as displayed in Table 2.
CONCLUSION
Differences in both ancillary
and medical treatment, found among Nigerian ophthalmologists in management of
closed globe traumatic hyphaema reflect situation among practitioners in
other parts of the world because of absence of clear cut protocol for
management derived from controlled trials. Difficulty in devising a controlled
trial in this condition include problem of adequately matching patients and
ethical considerations of study protocols in which no treatment controls are
utilized10. Many outcome studies of traumatic hyphaema management
were noted as flawed due to inadequate protocol and bias10,16
limiting their utility and validity as guide. The best that can be done is to
get data from a wide base of trained observers and practitioners who manage
this condition for a closer approximation to a valid guideline. This we have
attempted to do in this study resulting in some suggestions and recommendations
to act as a guide, although the application in some situations may need
modification as is usually advised in management of probably all medical
conditions.
Authors Affiliation
Dr. Okosa Michael Chuka
Senior Lecturer, and Former Head, Department of Ophthalmology
Nnamdi Azikiwe University and Consultant Ophthalmologist and former Head,
Guinness Eye Centre Nnamdi Azikiwe University Teaching Hospital; Onitsha,
Nigeria
Dr.
Onyekwe Lawrence Obizoba
Consultant Ophthalmologist Department of Ophthal-mology, Nnamdi
Azikiwe University Teaching Hospital and Guinness Eye Centre Onitsha, and Professor
of Ophthalmology, College of Health Sciences, Nnamdi Azikiwe University, Nnewi
campus, Nigeria
Dr. Anajekwu Cosmas Chinedu
Resident
Doctors Nnamdi Azikiwe University, Nnewi campus, Nigeria
Dr. Mbakigwe Chidi Fidelis
Resident Doctors Nnamdi Azikiwe
University, Nnewi campus, Nigeria
REFERENCES
1.
Walton W, Van Hagen S, Grigorian R, Zarbin M. Management of traumatic hyphaema. Surv Ophthalmol. 2002; 47:
297-334.
2.
Sheppard JD, Crouch ER, Williams PB, Crouch ER, Rastogi S,
Garcia-Valenzuela E. Hyphaema. http:// emedicine.medscape.com/article/1190165-overview.
3.
Luksza L, Homziuk M, Nowakowska Klimek M, Glasner L,
Iwaszkiewicz Bilikiewicz. Traumatic hyphaema
caused by eye injuries. B. Klin Oczna. 2005; 107: 250-1.
4.
Shiuey Y, Lucarelli MJ.
Traumatic hyphema: outcome of outpatient management. Ophthalmol. 1998; 105:
851-5.
5.
Fareed A, Warid M, Al Mansouri F. Management of non-penetrating traumatic hyphema in ophthalmology
department of HMC review of 83 cases. Middle East J of Emergency. 2004; 4: 1.
6.
Behbehani AH, Abdelmoaty
SMA, Aljazaf A. Traumatic hyphema Comparison
between different treatment modalities. Saudi J Ophthalmol. 2006; 20: 164-6.
7.
Rakusin W: Traumatic hyphema. Am J Ophthalmol 1972; 74: 284-92.
8.
Papaconstantinou D, Georgalas I, Kourtis N, Karmiris E,
Koutsandrea C, Ioannis Ladas I, Georgopoulos G. Contemporary aspects in the prognosis of hyphaema. Clin
Ophthalmol. 2009; 3: 28790.
9.
Yasuna E. Management of Traumatic
Hyphaema. Arch Ophthalmol. 1974; l 91: 190-91.
10.
Romano PE, Phillips PJ.
Traumatic hyphaema: a critical review of scientifically catastrophic history of
steroid treatment therefore; and a report of 24 additional cases with no
re-bleeding after treatment with the yasuna systemic steroid, no touch
protocol. Bin Vis Strab. 2000; 15: 187-96.
11.
Kelly JL, Blanquist PH.
Management of traumatic hyphema in Texas. Tex Med. 2002; 98: 56-61.
12.
Little BC, Aylward BW. The medical management of traumatic hypheama: a survey of opinion
among ophthalmologists in the UK. J Roy Soc Med. 1993; 86: 458-9.
13.
Earl R, Crouch ER Jnr.
Management of traumatic hyphaema: therapeutic options. J Paedtr Ophthlmol Strab.
1999; 36: 238-50.
14.
Oksala A. Treatment of traumatic
hyphaema. Br J Ophthalmol. 1967; 51: 315.
15.
Fong LP. Secondary hemorrhage in
traumatic hyphema. Predictive factors for selective prophylaxis. Ophthalmol.
1994; 101: 1583-8.
16.
Hopewell S, Loudon K, Clarke MJ, Oxman AD, Dickersin K. Publication bias in clinical trials due to statistical
significance or direction of trial results. Cochrane Database of Systematic
Reviews 2009, Issue 1.