Congenital cataracts account for 1
out of every 2000 live births,1 and are quite common, causing 10% of
all preventable visual loss in children globally.2 Pediatric
cataracts are responsible for more than 1 million childhood blindness in Asia.3
Visual loss is mainly due to stimulus deprivation amblyopia, strabismus
and nystagmus which are proportionately related to the size, location and
density of the opacity, especially if bilateral.4,5 Several
different classification systems exist including morphology, etiology, presence
of specific metabolic disorders, associated ocular anomalies or systemic
findings.1
Compared to adults, decision for
surgery is more difficult as subjective visual assessment in children cannot be
obtained, and surgeons rely largely on the morphology and location of the
cataract and behavior of the child. Surgery needs to be undertaken within the
first three months of life as indicated by experimental and clinical research,5
as early detection and management is directly related to the visual outcome.
Controversy6 still remains as regards to the age at which an IOL
can be safely implanted inside the eye. Aphakia management poses a significant
problem and needs spectacles or contact lenses. Success; however is directly
related to parental compliance and child cooperation. Results of pediatric
cataract surgery are based not only on the anatomic success but the
postoperative maintenance of a clear visual axis, and aggressive management of
pre-existing amblyopia and its prevention.
We embarked on this study, to observe
different morphologies of the congenital cataracts which presented to us, and
to manage them surgically, with appropriate visual rehabilitation, and to
assess the visual outcome after management.
MATERIAL
AND METHODS
A total of 46 eyes of 28 patients
presenting to Ophthalmology Department, Holy Family Hospital, Rawalpindi from
to 1st January, 2012 till 30th September, 2012 who were
diagnosed as congenital cataracts on the basis of morphology (any age), and
were operated during this period, were included in this study. Exclusion
criteria included trauma, uveitis, glaucoma, anterior segment abnormalities,
fundus abnormalities and systemic or syndromic associations. A detailed history
and physical examination was done, along with visual acuity assessment,
tonometry, slit lamp examination, retinoscopy, ophthalmoscopy, B-scan
ultrasonography, keratometry and Intraocular lens (IOL) power assessment by
SRK-II formula where necessary. The pupils were dilated with cyclopentolate 1%
or phenylephrine 10%. All patients were treated with lens aspiration with
anterior capsulorhexis via the limbal approach. Primary posterior capsulotomy with
anterior vitrectomy was done only in selected cases due to absence of an AC
maintainer in our hospital. Primary IOL implantation was done in children above
two years of age. All cases were treated with topical steroid-antibiotics for
at least 6 weeks. Cycloplegics or systemic steroids were needed in severe
postoperative inflammation. The patients were followed up at 1st
postoperative day, then 1st postoperative week, then monthly for at
least 3 months. Thereafter, follow up was variable, with the range between 3
months to 15 months. Visual acuity was done with Snellen chart in adults, the
picture Snellen chart in co-operative children, and fixation was noted in
smaller children. Data was analyzed using SPSS version 16. Frequencies and
percentages of age, gender, cataract morphology, and complications were noted.
Pre and post-operative visual outcome was assessed and Chi square test was
applied, with a p value less than 0.05 being considered significant.
RESULTS
A total of 46 eyes of 28 patients
ranging from 3 months to 25 years, with a mean age of 9.6 ± 8.1 years, were
included in this study. There were 16 (57.1%) females and 12 (42.8%) males.
Unilateral cataracts were seen in 3 (10.7%) patients only with bilateral
involvement in 25 (89.2%) patients. Consanguinity was present in 16 (57.1%)
patients. Morphologically, isolated lamellar cataract with riders was the most
common type found in 12 eyes (26.1%), along with total white cataract, also in
12 eyes (26.1%), followed by isolated blue dot cataract in 3 eyes (6.5%),
isolated nuclear, sutural and PSCO (posterior subcapsular cataract) in 2 (4.3%)
eyes each. A combination of different morphologies were found in 13 (28.2%)
eyes, with combined blue dot and sutural in 4 (8.7%) eyes, blue dot and PSCO in
3 (6.5%) eyes, nuclear and PSCO in 3 (6.5%) eyes, coronary and PSCO in 2 (4.3%)
eyes and combined lamellar and sutural cataract in 1 (2.2%) eye (Table 1) (Fig.
1).
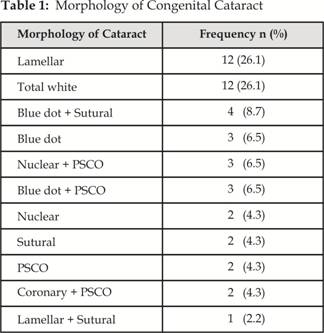
Fig. 1: Pie Chart of Congenital Cataract Morphology
Lens aspiration with Intraocular lens
(IOL) implantation was done in 31 (67.4%) eyes, Lens aspiration with anterior
capsulotomy alone, was performed in 13 (28.3%) eyes, and Lensectomy with
posterior capsulotomy and anterior vitrectomy was done in only 2 (4.3%) eyes due
to lack of an AC maintainer. IOL implantation was done in children above 2
years of age. Aphakic and uncooperative children required a secondary procedure
for posterior capsular opacification with surgical capsulotomy alone or
surgical capsulotomy with a secondary IOL later. Cooperative children and
adults were treated with Nd-YAG laser capsulotomies. Visual rehabilitation was
done in all patients, either with aphakic spectacles in children less than 2
years and residual refractive error was corrected with appropriate spectacles.
Patching was advised to the parents in case of children.
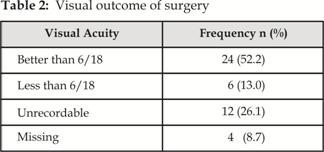
At presentation, visual acuity ranged
from light perception to 6/12, with only 13 (28.3%) eyes with visual acuity of
6/18 or better, 15 (32.6%) eyes had vision less than 6/18, and 18 (39.1%) eyes
had unrecordable vision. The postoperative best corrected visual outcome was
significantly improved (p= 0.000) ranging from unrecordable to 6/6, with 24
(52.2%) eyes having visual acuity of 6/18 or better (Table 2). 3 patients
were lost to follow up at 3 months.
Early complications included severe
inflammation in 22 (47.8%) eyes, mild inflammation in 13 (28.3%) eyes and
striate keratitis in 10 (21.7%) eyes. These were managed appropriately with
topical antibiotic-steroid combinations, cycloplegics and systemic steroids.
Late complications included Posterior capsular opacification (PCO) in 40
(86.9%) eyes, retinal detachment in 2 (4.3%) cases, pseudophakic glaucoma in 1
(2.2%) case, and persistent uveitis leading to phthisis bulbi in 1 (2.2%) case.
PCO was managed by surgical capsulotomies in children less than 4 years and
older patients were treated with Nd-YAG laser capsulotomy. The patients are
still on follow up and are part of a larger study.
DISCUSSION
Congenital cataract is a term used to
define lenticular opacities at birth. Infantile cataract encompasses all lens
opacities that develop within the first year of birth. The terms are used
interchangeably due to some of these opacities being missed at birth only to be
discovered later in life by ophthalmologists. They vary in severity from being
non-progressive and visually insignificant to causing profound visual
impairment.1
Bilateral congenital cataract
accounts for 15%7 of blindness in children worldwide. Idiopathic2,7
cataracts are the most common. Underlying and associated causes of congenital
cataract vary worldwide. Isolated hereditary cataracts account for 25% of
cases, the most common being autosomal dominant, then autosomal recessive or
X-linked.2,8 Down, Patau, Edward, Turner and Cri du chat syndromes
along with systemic diseases like galactosemia, Lowe, Fabry, Alport, Dystrophia
myotonica, hypoglycemia, hypoparathyroidism and Marfan syndrome are frequent
associations. Maternal infections like rubella, toxoplasma, cytomegalovirus,
herpes simplex and varicella (TORCH) may be causative.1,2,4,8,9
Morphologically cataracts may be
classified into fibre-based and non-fibre based. These include anterior or
posterior polar cataracts, lamellar (round, grey shell surrounding a clear
nucleus), nuclear or cataracta centralis pulverulenta, sutural or stellate,
floriform (flower – shaped), coralliform (coral-shaped), blue dot (punctate
cerulean cataract), coronary (supranuclear), subcapsular, total white,
disciform, oil-droplet, spear and membranous cataracts. Lamellar cataract is
the commonest.1,2,4,8,9,10
In our study, isolated lamellar and
isolated total white cataract were the most common, but combined patterns
accounted for the largest number of eyes. Other studies have shown lamellar,10
nuclear11 and total white12 cataracts to be the
commonest.
Visual loss in congenital cataract is
predominantly caused by amblyopia, which arises in a number of ways7:
stimulus – deprivation; competitive inhibition between the two eyes due to
unilateral or asymmetrical bilateral cataract; improper aphakia management; or
stimulus deprivation secondary to posterior capsular opacification. Thus
amblyopia reversal, treatment and prevention have profound long term
implications on the patient.
In unilateral cataract, clinical
observational studies have revealed that surgery by six to eight weeks7
has a better visual outcome as compared to later intervention. This may also be
the “critical period” for bilateral disease. Optimal timing for surgery is
difficult to establish due to the association of aphakic glaucoma with very
early surgery. Some have suggested that early IOL implantation may protect
against this complication.7,13
Despite significant improvements in
surgical, optical and visual rehabilitation techniques, an optimal surgical
approach is yet to be established. Several techniques are available like
lensectomy, anterior vitrectomy and/or combined with primary posterior
capsulotomy. Two main approaches exist for pediatric cataract removal: the limbal
approach and the pars plana approach, the latter being considered the most
versatile4. The anterior chamber maintainer (ACM) is considered
vital for pediatric cataract surgery. Anterior capsulorhexis, either manually
or with a vitrectomy probe, along with elective posterior capsulectomy and deep
anterior vitrectomy has been considered for infants under 2 years of age; above
2 years, this is considered optional.1,2,4,7,9,13 The pars plana
approach is indicated mainly for infants less than 2 years of age, particularly
with bilateral cataracts. Simultaneous surgery reduces the risk of relative
amblyopia which may occur even when few days apart.4
IOL implantation has been advocated
in children two years2 and above, due to problems arising due to IOL
power, size, availability, material, refraction change and long term IOL safety.6
However, many ophthalmologists now implant IOLs in younger age groups like one
year with successful outcomes.14-16 IOL power should be under
corrected by 20% in children less than 2 years, and in children between 2 and 8
years, under corrected by 10%.4,9 The postoperative residual
refractive error is corrected with spectacles. Pediatric IOLs should be in the
range of 10.5-12mm ideally17. Techniques of IOL placement
include in-the-bag, ciliary sulcus or IOL optic placement behind the capsular
bag.18 Hydrophilic acrylic IOLs have fewer postoperative
complications15 as compared to rigid PMMA lenses. Heparin coated7
PMMA IOLs reduce postoperative uveitis. In our study, we implanted either hydrophilic
acrylic or rigid PMMA IOLs, with comparable results.
Pediatric eyes are especially prone
to complications like fibrinous anterior uveitis, posterior capsular
opacification, lens reproliferation (Soemmerring ring), secondary pupillary
membranes, aphakic or pseudophakic glaucoma in 25% (often years later),
endophthalmitis, retinal detachment (also late) and unpredictable final
refraction.1,2,4,6,7,8,9,13,19
The visual outcome depends on
cataract type, timing of intervention, quality of surgery, and above all,
amblyopia management. Poor visual outcome with refractory amblyopia is
associated with dense cataracts, unilateral cataracts, late presentation to the
ophthalmologist, and poor compliance to occlusion therapy20.
Bilateral cataracts have been associated with a lesser risk of refractory
amblyopia. Dense, central, large and posterior cataracts lead to early
amblyopia, and a subsequent poor visual outcome. Partial, less dense, anterior,
and smaller cataracts even if detected late, can be managed effectively with a
good visual outcome21. In our study, most lamellar cataracts
although detected late, resulted in very good post-operative vision.
Limitations of our study were many.
This is not a study on pediatric patients alone and to evaluate morphology, we
included older patients as well. Lack of an ACM prevented us from managing
children less than 2 years of age appropriately with a primary posterior
capsulotomy and anterior vitrectomy and only irrigation and aspiration was
done, which resulted in early PCO formation, necessitating surgical
capsulotomies and increasing the number of surgical procedures for every
patient.
Final visual outcome in children was
poorer as compared to older patients, due to poor parental compliance with
spectacles, patching and follow up. Appropriate management of congenital
cataract in a developing country poses a lot of problems both for the doctors
and the patients. Lack of essential equipment, together with illiteracy,
poverty and irregular follow up affect tremendously the management of such
cases. Late presentation of children to hospitals results in refractory
amblyopia. Unaffordability of contact lenses, poor compliance with aphakic
glasses and reluctance to patching all contribute to poor postoperative visual
outcomes in aphakic children. Similarly in children who present later and are
implanted IOLs, refractory amblyopia is difficult to reverse and owes mostly
due to poor compliance of patching. However, partial cataracts even when
detected later, when treated, yield good results with much patient and doctor
satisfaction.
Early diagnosis and management along
with parental advice and support is the key to successful visual
rehabilitation. Strategies to screen and detect congenital cataract within the
first three months of life are needed for early diagnosis and routine ocular
examination5 of neonates and young infants should be done routinely
by ophthalmologists to prevent late detection and subsequent poor visual
outcome.
CONCLUSION
Congenital cataract varies
considerably in morphological appearance with the major types being lamellar,
total white, combined pattern and blue dot. Early surgical management with
aggressive postoperative rehabilitation and amblyopia therapy is essential for
effective visual outcome. Visual outcome is better for partial, bilateral
cataracts as compared to total white or unilateral cataracts.
Author’s Affiliation
Dr. Sana Nadeem
Senior Registrar
Ophthalmology Department
Fauji Foundation Hospital, Rawalpindi
Dr. Muhammad Ayub
Senior Registrar
Ophthalmology Department
Holy Family Hospital, Rawalpindi
Dr. Humaira Fawad
Consultant Ophthalmologist
Ophthalmology Department
District Headquarters Hospital, Rawalpindi
REFERENCES
1.
Rosenfeld
SI, Blecher MH, Bobrow JC, Bradford CA, Glasser D, Berestka JS. Lens and
Cataract. Section 11. Basic and Clinical Science Course. American Academy of
Ophthalmology. San Francisco. 2005; 33-9.
2.
Simon JW,
Buckley EG, Drack AV, Hutchinson AK, Plager DA, Rabb EL, Ruttum MS, Aaby AA. Paediatric
Ophthalmology and Strabismus. Section 6. Basic and Clinical Science Course.
American Academy of Ophthalmology. San Francisco. 2005; 277-89.
3.
World
Health Organisation. Prevention of childhood blindness. Geneva: WHO; 1992.
4.
Yanoff M,
Duker JS. Ophthalmology. Second Edition. Mosby: St Louis.
2004; 279-379.
5.
Rahi JS, Dezateux C. National cross
sectional study of detection of congenital and infantile cataract in the United
Kingdom: role of childhood screening and surveillance. The British Congenital
Cataract Interest Group. BMJ. 1999; 318: 362-5.
6.
Javadi MA. Pediatric
cataract surgery. Editorial. J Ophthalmic Vis Res. 2009; 4: 199–200.
7.
Wormald R, Henshaw K, Smeeth L. Evidence-Based
Ophthalmology. London: BMJ
Publishing group; 2008. www.books.google.com. 2012; 47-51.
8.
Kanski JJ,
Bowling B. Clinical Ophthalmology. A systematic approach.
Seventh Edition. Elsevier: London. 2011; 298-304.
9.
Denniston
AKO, Murray PI. Oxford handbook of ophthalmology. Oxford
University Press: Karachi. 2007; 235-627.
10. Jain IS,
Pillay P,
Gangwar DN,
Dhir SP,
Kaul VK. Congenital
cataract: etiology and morphology. J Pediatr
Ophthalmol Strabismus. 1983; 20: 238-42.
11. Wilson ME, Trivedi RH, Morrison DG, Lambert SR,
Buckley EG, Plager DA et al. The Infant Aphakia Treatment Study: evaluation of
cataract morphology in eyes with monocular cataracts. J AAPOS. 2011; 15: 421-6.
12. Kaid
Johar SR, Savalia NK, Vasavada AR, Gupta PD. Epidemiology based etiological study of pediatric cataracts
in Western India. Indian J Med Sci. 2004; 58: 115-21.
13. Mazhar-ul-Hasan, Qidwai UA,
Aziz-ur-Rehman, Bhatti N, Alvi RH. Complication and visual outcome
after pediatric cataract surgery with or without Intraocular
lens implantation.
Pak J Ophthalmol. 2011; 27: 30-4.
14. Yorston
D. Intraocular
lens implants in children. J Comm Eye Health. 2001; 14: 57-8.
15. Rowe
NA, Biswas S, Lloyd IC.
Primary IOL implantation in children: a risk analysis of foldable acrylic v
PMMA lenses. Br J Ophthalmol. 2004; 88: 481-5.
16. Flicroft
DI, Knight-Nanan D, Bowell R, Lanigan B, O’Keefe M. Intraocular lenses in children:
changes in axial length, corneal curvature, and refraction. Br J Ophthalmol. 1999; 83: 265–9.
17. Bluestein EC, Wilson ME, Wang XH, Rust PF, Apple DJ. Dimensions of the pediatric crystalline lens: implications for
intraocular lenses in children. J Pediatr Ophthalmol Strabismus. 1996; 33: 18-20.
18. Gimbel HV, DeBroff BM. Posterior capsulorhexis with optic capture: maintaining a clear visual
axis after pediatric cataract surgery. J Cataract Refract
Surg.
1994; 20: 658-64.
19. Speeg-Schatz C. Results and complications of
surgery of congenital cataract. [Article in French] J Fr Ophthalmol.
2011; 34: 203-7.
20. Harrad R. Modulation of amblyopia therapy
following early surgery for congenital cataracts. Br J Ophthalmol. 1995; 79: 793.
21. Ondráček O, Lokaj M. Visual
outcome of congenital cataract surgery. Long term clinical results. Scripta
Medica. 2003; 76: 95-102.