Cataract
affects approximately 20 million people worldwide and this figure is expected
to reach 50 million by the year 20201. In Pakistan
cataract accounts for 66.7% of the total blindness2 and cataract
surgery is the most commonly performed ocular surgery3.
Small
incision cataract surgery doesn’t require suturing of wound, has low risk of
intra operative and postoperative complications and results in rapid visual
rehabilitation4. Phacoemulsification results in better postoperative
visual acuity (VA) than extra capsular cataract extraction (ECCE) at all
postopera-tive intervals5. Therefore, phacoemulsification is almost
universally preferred nowadays6.
Spectacles
or contact 5 lenses can be used to correct astigmatism. Spectacles wear for
correction of astigmatism can cause various optical aberrations. Contact lens wear
has a number of side effects such as risk of infection, mechanical and hypoxic
keratitis, immune response keratitis and giant papillary conjunctivitis7.
Correction
of preexisting astigmatism simultane-ously with cataract surgery is attempted
nowadays. Different methods of reducing astigmatism during cataract surgery
include keratotomy, toric intraocular lens (IOL) implantation, opposite clear
corneal incision (OCCI) and limbal relaxing incisions or corneal relaxing
incisions5.
A clear
corneal incision given during phaco-emulsification at the steep meridian of
cornea 8,9. Limbal
relaxing incisions performed during phacoemulsification are also very safe,
stable and effective in reducing pre-existing corneal astigmatism9.
The objective of the study was
to determine the mean change in pre-existing astigmatism, by site of incision
in phacoemulsification as altering the incision site may help in reducing
pre-existing astigmatism.
MATERIAL AND METHODS
It was
a prospective study conducted at Ophthal-mology Department, Khyber Teaching
Hospital Peshawar, from March 1st
2012 to August 31st 2012. All patients with age related
cataract with pre existing astigmatism of 1D or more were included in the
study. Patients having irregular astigmatism and astigmatism due to pterygium,
previous history of any surgery in same eye, corneal opacity and those having
traumatic or complicated cataract were excluded from the study. Sampling
technique was non-probability consecutive sampling.
Approval
was taken from the hospital ethical committee before starting the study and
written informed consent was taken from the patients. Pre-operatively detailed
history was taken and complete systemic and ocular examination was done,
including keratometry for the type and degree of astigmatism.
All
cases were operated by phacoemulsification with IOL implantation keeping 3.2mm
incision at the limbus perpendicular to steep meridian of cornea. After
viscoelastic material was injected, a continuous curvilinear capsulorhexis,
hydro dissection, phaco-emulsification, aspiration of cortex and capsular bag
refilling with viscoelastic solution was performed. A foldable acrylic IOL was
implanted in the capsular bag. Viscoelastic material was removed and anterior
chamber formed with Ringer’s lactate. Wound was tested for water tightness. In
all eyes phaco power, viscoelastic gel, irrigation solution (Ringer’s lactate)
and IOL were kept constant. All surgeries were performed by the same surgeon.
Postoperatively
each patient received 0.3% ofloxacin eye drops and 0.1% dexamethasone eye drops
4 times / day. Steroid eye drops were tapered in 4 – 6 weeks. Analgesics were
used whenever required.
Post-operatively the patients
were followed up after 6 weeks. At follow up visit, keratometry was performed
to see the effect of incision site in the form of correction of pre-existing
astigmatism. All the relevant data was recorded in a pre-designed proforma. All
the collected data was analyzed using SPSS version 10.0.
RESULTS
The
number of patients included in our study was 113. Patient’s age ranged from
41 to 84 years with a mean of 59.36 ± 10.08 years. 62 patients (54.86 %)
were male and 51 (45.13%) were female. All the patients underwent
phacoemulsification and IOL implantation through a 3.2 mm wide incision
perpendicular to the steep meridian of cornea. Right eye was operated in 59
(52.21%) cases and left eye was operated in 54 (47.78%) cases.
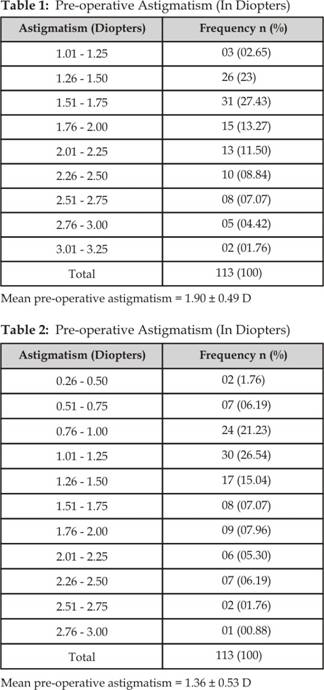
Pre-operative astigmatism in all the patients was measured in
diopters (Table 1). The mean pre-operative astigmatism was 1.90 ± 0.49 diopters
with a range from 1.20 to 3.25 diopters.
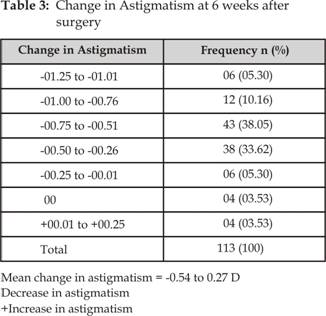
All
patients were followed up at 6th week post-operatively and
post-operative astigmatism was recorded (Table 2). The mean post-operative astigmatism
was 1.36 ± 0.53 diopters with a range from 0.50 to 2.80 diopters.
Difference
between pre-operative and post-operative astigmatism was noted at 6 weeks
(Table 3). The change in astigmatism was ranging from -1.25 D to + 0.25
diopters with a mean of -0.54 ± 0.27 diopters. The astigmatism decreased in 105
eyes (92.92%), remained unchanged in 4 eyes (3.53%) and increased in 4 eyes
(3.53%). The mean change in astigmatism at the end of my study was 0.54 ± 0.27
diopters. Student t test was applied for significance of change in astigmatism
after the surgery. The p value was 0.0001 and this
difference was considered to be statistically significant.
DISCUSSION
Modern
cataract surgery aims at achieving a good refractive outcome postoperatively
with minimal post-operative astigmatism10. Postoperative astigmatism
depends on the site, width and architecture of the incision and suturing
technique11,12. Even with small incision cataract surgery using
foldable IOL the visual outcome may vary greatly due to pre-existing
astigmatism.
Placing
the incision on the steepest meridian results in decreased refractive power in
that meridian and an increased refractive power in the meridian perpendicular
to it13. In our study this concept was utilized in eyes with
pre-operative astigmatism of 1.00 D or more. In this study a 3.2 mm
self-sealing incision was given perpendicular to the steep axis of cornea to
assess the effect of a site of incision on neutralizing the pre-existing
astigmatism.
This
study shows that by placing a 3.2 mm incision perpendicular to the steeper
axis, it is possible to reduce the amount of astigmatism in eyes with
pre-operative astigmatism of 1.00 D or more. Lever and Dahan14
reported in their study that a 3.5 mm opposite clear corneal incision in the
steep meridian was effective in reducing pre-existing corneal astigmatism by a
mean value of 2 Diopters.
Corresponding
figures have been reported to be 0.5 Diopters by Tadros15 and 1.5
Diopters by Khokhar.8 In one study,16 in patients who underwent
conven-tional small incision cataract surgery (SICS), eyes with superior
incisions had 1.92 ± 0.53 D “against the rule” astigmatism and eyes with
temporal incisions had 1.57 ± 0.24 D “with the rule” astigmatism at 90 days. In
patients who underwent phacoemulsification, 1.08 ± 0.36 D astigmatism was seen
with clear corneal incision and 1.23 ± 0.71 D astigmatism was seen with
corneo-scleral incision. In the study of George et al17, mean
astigmatism after conventional ECCE, manual SICS and phacoemulsification
surgery was 1.77 D, 1.17 D and 0.77 D respectively (P = 0.001).
In our
study a 3.2 mm clear corneal incision was given in all cases, in the steep
meridian. Post-operative keratometry was done 6 weeks after the surgery, to
give time for complete wound healing and stabili-zation of refraction. The
decrease in astigmatism at the follow up was 0.54 ± 0.27 diopters. The difference between pre-operative and post-operative
astigmatism was statistically significant (P value = 0.0001). However, placing the corneal incision in the steep
meridian alone may not fully correct high astigmatism and this may have to be
combined with other procedures5 or the residual astigmatism may have
to be corrected with glasses post-operatively.
CONCLUSION
A 3.2
mm wide incision for phacoemulsification placed perpendicular to steep axis of
cornea is effective in reducing the pre-existing
corneal astigmatism.
Author’s Affiliation
Dr. Akbar Khan
Eye Surgeon
Khyber
Eye Foundation, Peshawar
Dr. Mumtaz Alam
Senior Registrar
Ophthalmology Department
Kuwait
Teaching Hospital, Peshawar
Dr. Muhammad Rafiq Afridi
Assistant Professor
Ophthalmology Department
Rehman
Medical Institute, Peshawar
Dr. Imran Ahmad
Medical Officer
Khyber Teaching Hospital, Peshawar
REFERENCES
1.
Zaman M,
Iqbal S, Khan YM, Khan MT, Jadoon MZ, Qureshi MB, Safi MA, Khan MD. Manual
small incision cataract surgery (MSICS). Review of first 500 cases operated in
microsurgical training center. Pak J Ophthalmol. 2006; 22: 14-22.
2.
Khan AQ,
Qureshi B, Khan MD. Rapid assessment of cataract blindness in age 40 years and above
in District Skardu, Baltistan, Northern Areas of Pakistan. Pak J Ophthalmol.
2003; 19: 84-9.
3.
Qazi ZA. Corneal
endothelium tissue that demands respect. Pak J Ophthalmol. 2003; 19: 1-2.
4.
Ahmad A,
Ahmad J. Combined phacoemulsification, intraocular lens implantation and
trabeculectomy. Pak J Ophthalmol. 2000; 16: 26-8.
5.
Yi DH,
Sullivan BR. Phacoemulsification with indocyanine green versus manual
expression extracapsular cataract extraction for advanced cataract. J Cataract
Refract Surg. 2002; 28: 2165-9.
6.
Chakrabarti
A, Singh S. Phacoemulsification in eyes with white cataract. J Cataract
Refract Surg. 2000; 26: 1041-7.
7.
Kanski
JJ. Cornea. In: Kanski JJ Clinical Ophthalmology. A systemic approach
7th ed. Butterworth Heinemann Elsevier 2007; 167-238.
8.
Khokhar S, Lohiya P, Murugiesan V, Panda A. Corneal astigmatism correction with opposite clear corneal
incisions or single clear corneal incision: Comparative analysis. J Cataract
Refract Surg. 2006; 32: 1432-7.
9.
Altan – Yaycioglu
R, Akova YA,
Akca S,
Gur S, Oktem C. Effect
on astigmatism of the location of clear corneal incision in phacoemulsification
of cataract. J Cataract Refract
Surg. 2007; 23: 515-8.
10.
Rainer
G, Menapace R, Vass C. Corneal shape changes after temporal and superolateral 3.0 mm
clear corneal incisions. J Cataract Refract Surg. 1999; 25: 1121-6.
11.
Roman
SJ, Auclin FX, Chong-Sit DA, Ullern MM. Surgically induced astigmatism
with superior and temporal incisions in cases of with-the-rule preoperative
astigmatism. J Cataract Refract Surg. 1998; 24: 1636-41.
12.
Simsek
S, Yasar T, Demirok A, Cinal A, Yilmaz OF. Effect of superior and
temporal clear corneal incisions on astigmatism after sutureless
phacoemulsification. J Cataract Refract Surg. 1998; 24: 515-8.
13.
Elkington AR, Frank HJ, Greaney MJ. Refractive surgery. In:
Clinical Optics. 3rd edition. 1999; 242-54.
14.
Lever J,
Dahan E. Opposite clear corneal incision to correct preexisting
astigmatism in cataract surgery. J Cataract Refract Surg. 2000; 26: 803-5.
15.
Tadros
A, Habib M, Tejwani D, Lany HV, Thomas P. Opposite clear corneal
incisions on the steep meridian in
phacoemulsification: early effects on the cornea. J Cataract Refract
Surg. 2004; 30: 414-7.
16.
Reddy B,
Raj A, Singh VP. Site of incision and corneal astigmatism in conventional SICS
versus phacoemulsification. Ann Ophthalmol. 2007;
39: 209-16.
17.
George R, Rupauliha P, Sripriya AV, Rajesh PS, Vahan PV, Praveen
S. Comparison of endothelial cell
loss and surgically induced astigmatism following conventional extracapsular
cataract surgery, manual small – incision surgery and phacoemulsification. Ophthalmic Epidemiol. 2005; 12: 293-7