A group
of diseases mimicking intraocular inflammation and uveitis are termed as
masquerade syndrome,1 which may be classi-fied as benign or
malignant. Sympathetic ophthalmia is an autoimmune granulomatous intra-ocular
inflammation occurring most commonly within one year of surgery or trauma2.
The injured eye termed as the excited eye while the fellow eye that develops
inflammation without any obvious reason is called as sympathizing eye.
Retinoblastoma
is the most common pediatric intraocular tumor occurring classically prior to 5
years of age. It usually presents as leukocoria, strabismus or decreased
vision. Only 1 – 3% present of retinoblas-tomas present as intraocular
inflammation3.
We present as case report of a
6 year old girl in which retinoblastoma presented as sympathetic ophthalmia,
thus masquerade syndrome.
CASE REPORT
A six year old female child
first presented with chief complaint of painful loss of vision in her right eye
(OD) for a few days after trauma with stick. On examination her OD had large
hyphema with markedly raised intraocular pressure (IOP) (Fig. 1.A) and left eye
(OS) was within normal limits. Paracentesis of OD was done and blood was sent
for gram staining and culture, which revealed no growth or micro-organism. Two
months later the child presented with complaint of no vision in her OD and
painful reduced vision and photophobia in OS. Her general health was good with
no history of fever and review of systems was normal. On examination her visual
acuity (VA) was no perception of light (NPL) in OD and not recordable in OS due
to photophobia. On slit lamp examination her OS had multiple keratic precipitates,
cells in anterior chamber (AC) and vitreous, posterior synchiae, fundus view
was hazy (Fig. 1.B). Her baseline investigations, x-ray chest and B-scan of OS
were normal. Based on these findings patient was provisionally diagnosed as a
case of sympathetic ophthalmia, her OD being the excited eye and OS the
sympathetic eye which developed uveitis without any obvious etiology other than
the trauma to the OD. She was kept on systemic and topical steroids prior to
proceeding for enucleation of OD. Following the enucleation the OS became quiet
(Fig. 1.C) and the child was sent home. To our surprise the histopathology
report of the enucleated eye concluded it to be a Retinoblastoma (RB). Since
the child’s history was not suggestive of RB and her age was old for RB we
requested the laboratory to review the slides again. A board of pathologists
reviewed the slides, concluding that it was a RB indisputably showing well
differentiated Homer - Wright rosettes and Flexener - Wisternsteiner rosettes
(Fig. 2). On TNM staging patient had a pT2 Nx Mx with no optic nerve
involvement. Patient was referred to an advance oncology unit for further
management of RB.
Fig. 1: (A) Right eye on first
presentation showing hyphema, anterior staphyloma. (B) Left eye at second visit
showing keratic precipitates, posterior synchiae (C) Post enucleation right eye
with prosthesis and left eye is normal
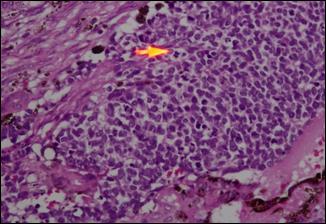
Fig. 2: Histopathological slide
of enucleated right eye, arrow showing mitotic figures.
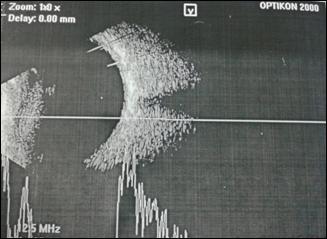
Fig. 3: Normal ultrasound B - Scan
of left eye after enucleation of right eye

Fig. 4: CT Scan of brain and
orbit done after enucleation, showing implant in right eye and normal left eye.
DISCUSSION
Masquerade
syndrome is a rare entity as it presents an unusual presentation of relatively rare
conditions; therefore mostly they are either undiagnosed or under diagnosed.
They may be benign or malignant; however the latter are more common. Some of
the malignant masquerading conditions include primary intraocular lymphoma,
uveal melanoma, retinoblas-toma, leukemia, metastatic lesions and
paraneoplastic syndromes.1 Uveitis in the pediatric population is
less common than adults. A British study reported the incidence of pediatric
uveitis to be 3.15 per 100,000 children up to 5 years of age4.
The literature
does not give the actual incidence of sympathetic ophthalmia (SO), as it is a
rare condition but most studies concur that it is 0.2% to 0.5% following ocular
trauma and comprises only 0.3% of all uveitis2. The treatment
protocol is mainly medical comprising of corticosteroids or immuno-suppressive
therapy. Enucleation remains a debatable topic in SO: studies suggest primary
enucleation done within 10 days of injury, is beneficial for reducing the
inflamma-tion in the sympathetic eye. But it is quite difficult to give a
definite time frame for enucleation especially if the patient is a child. In
our case we performed a secondary enucleation as the excited eye was a painful
blind eye5 and the fellow eye developed refractory uveitis, which
resolved following the surgery.
Less than 10% of
retinoblastomas (RB) present as intraocular inflammation and 50% of these
present as orbital cellulitis6. Any other presentation makes the
already difficult diagnosis next to impossible, accounting for the majority of misdiagnosed
RBs. Our case did not have a typical presentation of RB, she had no relevant
family history and she had passed the age of usual RB which is mostly diagnosed
prior to 5 years of age6. The definite diagnosis can only
be reached after a histopathological evidence as was in our case.
CONCLUSION
Our case highlights a rare and
unique presentation of retinoblastoma as sympathetic ophthalmia, thus
masquerade syndrome. Any refractory uveitis particularly in a child should
raise a high index of suspicion of a masquerade syndrome and should be
evaluated thoroughly.
Author’s Affiliation
Dr. Noor Bakht Nizamani
Department of Ophthalmology, Liaquat University of Medical
& Health Sciences, Jamshoro/Hyderabad, Pakistan
Dr. Khalid Iqbal Talpur
Department
of Ophthalmology, Liaquat University of Medical and Health Sciences, Jamshoro /
Hyderabad, Pakistan
Dr. Sajjad Ali Surhio
Department of Ophthalmology, Liaquat
University of Medical & Health Sciences, Jamshoro / Hyderabad, Pakistan
REFERENCES
1.
Trzaska K, Romanowska – Dixon B.
Malignant uveitis masquerade syndromes. Klin Oczna. 2008; 110: 199-202.
2.
Arevalo JF, Gracia RA, Al-Dhibi HA, Sanchez JG, Suarez-Tata L. Update on sympathetic ophthalmia. Middle East Afr J Ophthalmol.
2012; 19: 13-21.
3.
Català-Mora J, Parareda – Salles
A, Vicuña-Muñoz Cg, Medina-Zurinaga M, Prat – Bartomeu J. Uveitis masquerade syndrome
presenting as a diffuse retinoblastoma. Arch Soc Esp Oftalmol. 2009; 84: 477-80
4.
Edelsten C, Reddy MA, Stanford MR, Graham EM. Visual loss associated with pediatric uveitis in English primary
and referral centers. Am J Ophthalmol. 2003; 135: 676-80.
5.
Savar A, Andreoli MT, Kloek CE, Andreoli CM. Enucleation for open globe injury. Am J Ophthalmol. 2009; 147:
595-600.
6.
Tsai T, O'Brien JM. Masquerade syndromes: malignancies mimicking
inflammation in the eye. International
ophthalmology clinics. 2002; 42:
115-31.