Original Article
Sight Threatening Diabetic
Retinopathy in Type 2 Diabetes Mellitus
Mohammad Memon, Sajjad Ali Surhio, Shahzad
Memon, Noor Bakht Nizamani, Khalid Iqbal. Talpur
Pak J Ophthalmol 2014, Vol. 30 No.
1
. . . .
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
. . . . . . . . . . . . . . . . .. . .. . . . . . . . . . . . . . . . . . . . .
. . . . . . . . . . . . . . . .
|
See
end of article for authors
affiliations
..
.. Correspondence
to: Noor Bakht Nizamani, Department of Ophthalmology, Liaquat University Eye Hospital, Jail Road, Hyderabad, 71000,
Sindh,
..
.. |
Purpose: To determine the
proportions of Proliferative Diabetic Retinopathy (PDR) and Clinically
Significant Macular Edema (CSME) in patients with known type2 Diabetes
Mellitus. Material
and Methods: A prospective study was conducted at Ophthalmology
Department, Liaquat University of Medical and Health Sciences, Hyderabad,
Pakistan. Duration of study
was one year, starting from 1st January 2010 till 31st
December 2010. Two hundred consecutive
type 2 diabetics diagnosed with diabetic retinopathy were classified
according to the most severe changes in the worse eye into the following
three stages based on EDTRS classification. 1) Patients with
NonProliferative Diabetic Retinopathy (NPDR). 2) Patients with CSME stage
(in the presence of NPDR). 3) Patients with PDR stage (irrespective of
presence or absence of CSME). Results:
The mean age of patients with diabetic retinopathy was 51.7 ±
9.4 years. 62 (31%) patients had PDR, and another 66 (33%) patients had CSME.
51.6% of patients with PDR were in the age group of 40 49 years and 56% of
patients with CSME were 50 59 years. Patients presented with PDR were
significantly younger (Pvalue < 0.001) than patients with CSME and NPDR.
51% of patients had DM for 15.7 ± 6.1 years; with a mean age of 30.5 ± 4.6
years at diagnosis with type 2 DM. Conclusion: 64% of
patients had sight threatening stages of diabetic retinopathy, and 34.4% of
them were 40 49 years of age. |
Diabetes Mellitus (DM) is a chronic, costly and potentially
disabling disease due to its severe complications. There are 285 million adults
worldwide with DM; having a prevalence of 6.4% among adults aged 20 79 years.1
Pakistan has the 7th largest population of DM with 7.1 million
people; having a prevalence of 9% among adults ≥ 25 years of age1,2.
Diabetic retinopathy is one of the common micro- vascular
complications of DM. The risk of developing diabetic retinopathy increases with
the duration of DM. 3 The prevalence of diabetic retinopathy among
diabetic subjects varies between 15.3% and 28.9% in various studies conducted
in Pakistan4,5.
Diabetic retinopathy progresses from the asymp-tomatic
Non-Proliferative Diabetic Retinopathy (NPDR); characterized by increased
vascular per-meability and progressive vascular closure, to the sight
threatening Proliferative Diabetic Retinopathy (PDR); characterized by growth
of new blood vessels on the retina3,6.
The new blood vessels in PDR may bleed causing vitreous hemorrhage
with sudden loss of vision, or may lead to tractional retinal detachment and
neovas-cular glaucoma. Meanwhile; Clinically Significant Macular Edema (CSME)
can develop during any stage of diabetic retinopathy, and it is characterized
by retinal thickening from leaky blood vessels causing slow and gradual
blurring of vision3,6.
More than 90% of cases of diabetes worldwide are type 2 DM. Type
2 DM occurs at a relatively younger age in the Indian Subcontinent than
elsewhere in the world7. Basit et al8 in a study on 2199
type 2 diabetics had observed that; the age at onset of DM was < 40 years
in 46.3% of type 2 diabetics.
Early onset type 2 DM may cause diabetic retinopathy to develop
at a relatively younger age. The aim of this study was to determine the
proportions of Proliferative Diabetic Retinopathy (PDR) and Clinically
Significant Macular Edema (CSME) in patients with known type 2 DM.
MATERIAL AND METHODS
This cross sectional study was carried out at Department of Ophthalmology,
Liaquat University of Medical and Health Sciences, Hyderabad, Pakistan, from 1st
January 2010 to 31st December 2010. The sample size was calculated
using computer software Open Epi Version 2. A sample of 200 diabetics with
retinopathy was required for 15.3% prevalence at 95% confidence interval and
absolute precision of ± 5% (based on 15.3% prevalence of diabetic retinopathy
in the diabetic subjects of the Pakistan National Blindness and Visual
Impairment Survey)4.
Diabetic retinopathy screening was performed in all known as well
as newly diagnosed type 2 diabetics (already on oral hypoglycemic drugs or on
insulin) coming to our hospital for routine checkup with or without complain of
decreased vision or any other ocular symptom.
Detailed history was taken including name, age, gender, duration
of DM and the mode of treatment (oral hypoglycemic drugs or insulin). Detailed
ocular examination was performed including best corrected visual acuity (BCVA),
anterior segment examination and fundus examination. Patients were excluded if
fundus details were not visible due to cataract or corneal opacity.
The patients were divided according to the most severe diabetic
retinopathy changes in the worse eye into the following three groups based on
EDTRS classification: a) Patients with NPDR stage b) Patients with CSME stage
(in the presence of NPDR) c) Patients with PDR stage (irrespective of presence
or absence of CSME). Also; the patients were stratified according to their age into
the following five age groups: Below 30 years, 30 39 years, 40 49 years, 50
59 years and above 59 years of age.
The data was analyzed using SPSS version 11 software. The
Descriptive Statistics obtained were; the age distribution, the proportion of
various stages of diabetic retinopathy, and the distribution of stage of
retinopathy by the age of patients. The mean and standard deviation (SD) for
the age at presentation with diabetic retinopathy, the duration of DM, and the
estimated age at onset of DM were compared; between different stages of
diabetic retinopathy using one way ANOVA test. P Value < 0.05 was taken as
significant.
RESULTS
In this study; 200 consecutive type 2 diabetics diagnosed with
diabetic retinopathy were included. 121 (60.5%) patients had presented with an
ocular symptom, meanwhile; the remaining 79 (39.5%) patients were referred for
diabetic retinopathy screening by physicians.
Over 52% of our patients were females with mean age of 50.4 ± 9.7
years. Males were significantly older with mean age of 53.1 ± 8.8 years (P
value = 0.043). Males also had a significantly longer duration of DM (P value
< 0.001); the duration of DM in males was 14.6 ± 7.4 years, while females
had a mean duration of 11.9 ± 4 years.
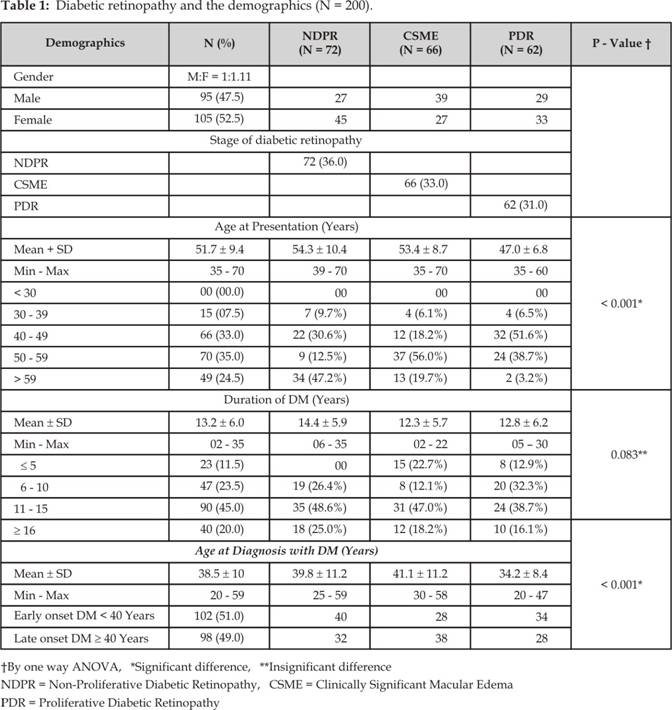
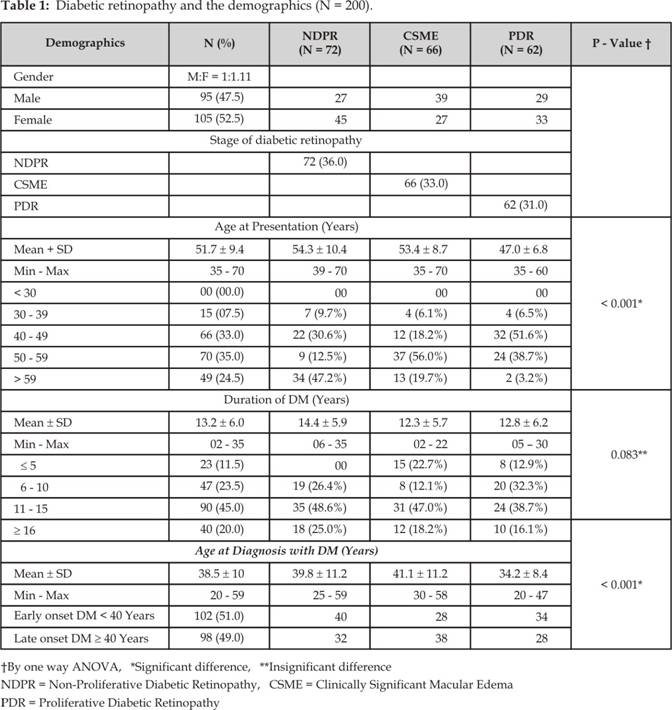
Table 1 shows the overall
demographic features of our patients along with difference in demographics of
patients with different stages of diabetic retinopathy.
The difference in the mean duration of DM in patients with
different stages of diabetic retinopathy was statistically insignificant (P
value = 0.083). However; patients with PDR were significantly younger at the
time of diagnosis with DM than other patients (P value < 0.001) (Fig. 1).
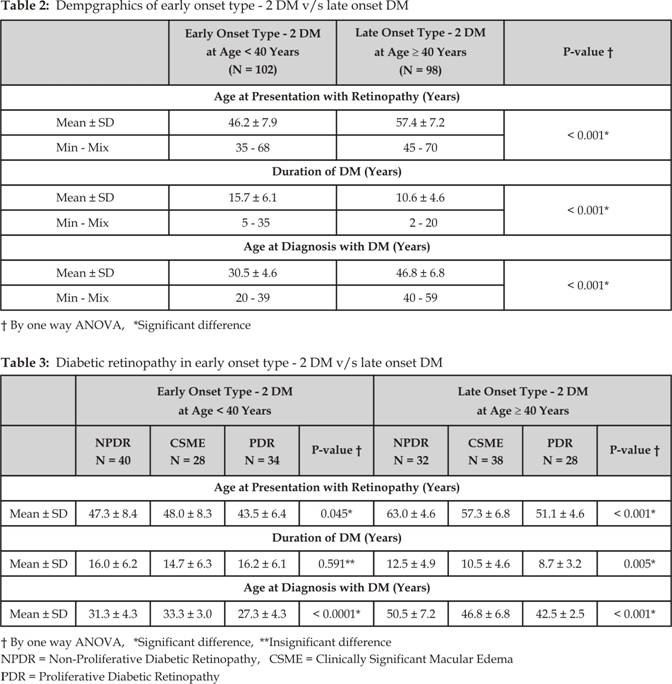
In 51% of patients the age at diagnosis with DM was < 40 years;
and they were considered to have early onset type 2 DM. 40.2% (41/ 102) of
patients with early onset type 2 DM had already been shifted from oral
hypoglycemic drugs to insulin by their physicians to control their DM.
Meanwhile; 17.3% (17 / 98) of patients with late onset type 2 DM were on insulin.
Because of early onset type 2 DM in our patients; 58.1% (36 /
62) of patients with PDR were < 50 years of age. Table 2 shows an overall comparison between patients with early
onset type 2 DM v/s late onset type 2 DM. Table 3 shows detailed comparison between patients with early
onset type 2 DM v/s late onset type 2 DM; presented with different stages
of diabetic retinopathy.
DISCUSSION
The prevalence and severity of diabetic retinopathy increases with
the duration of DM and age of the patients, along with; poor metabolic control;
But
traditionally; the age has been coupled to the duration of DM and was not
regarded as an independent risk factor3. Niazi et al9 and Chaudhary5
reported that only the longer duration of DM was proved to be an independent
risk factor for both type and progression of diabetic retinopathy. Al Maskari
and El Sadig10
observed an increase in the prevalence of diabetic retinopathy with increasing
age (P = 0.004) and disease duration (P = 0.0001). Similar results were
reported in several studies11,12.
In this study; the mean age of patients presenting with diabetic
retinopathy was 51.7 ± 9.4 years, which is consistent with other national5,1315, and
international studies11,1618.
Thirty one percent of our patients had the sight - threatening PDR, and similar
results were reported in literature2,13,14,1618.
Meanwhile, other studies had reported lower prevalence of PDR among patients
with any type of diabetic retinopathy, i.e. 11.7% (111 / 946) was reported by Chaudhary
GM5, 20.9% (163 / 780)
by Khan AJ15, and
14.6% (172 / 1176) was reported by Agrawal et al11. This lower prevalence of PDR might be related to
the difference in the duration of DM. The short duration of ≤10 years of
DM; was observed in 60.5% by Chaudhary GM5,
in 52.2% by Khan AJ 15,
and in 42.4% by Agrawal et al11.
Whereas in this study, only 35% of patients had DM for ≤10 years.
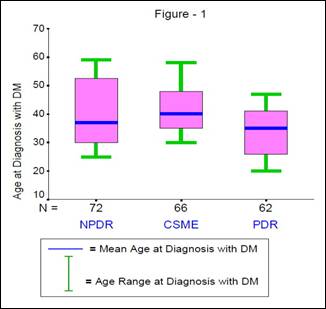
Fig. 1: Diabetic retinopathy
and age at diagnosis with diabetes mellitus
The prevalence of the sight threatening CSME among our patients
with NPDR was 47.8% (66/138), this is consistent with literature12,14,18,19.
However lower prevalence of CSME (15-22%)16,20 has been reported
among patients with NPDR, which could be related to the difference in the
duration of DM. In the aforementioned studies 53.7%20 and 49.6%16
patients had ≥ 11 years duration of DM, while 65% of our patients had
that much duration, which might explain the higher prevalence of CSME with
NPDR. The sight threatening diabetic retinopathy (either PDR or CSME) was
observed in 64% (128/200) of our patients. This high prevalence may be due to
the selection bias, and; it is one of the disadvantages of a tertiary hospital
based study like ours.
The mean age of our patients with CSME was 53.4 ± 8.7 years, and;
56.0% of them were 50 59 years, while; 18.2% were 40 49 years. Similarly;
Aziz-ur-Rahman et al 21 had reported that; 41.5% (34/82) of patients
with diabetic maculopathy were 51 60 years and 30.5% (25/82) were 41 50
years of age. Meanwhile; the mean age of our patients with PDR was 47.0 ± 8.8
years with 58.1% being < 50 years of age, which is younger age comparatively15.
We observed that, 51% of our patients with diabetic retinopathy
had early onset type 2 DM (< 40 years of age at diagnosis with DM), and
among them; 33.3% had presented with PDR, and another 27.5% had CSME. The trend
of early onset type 2 DM in Pakistan had been reported previously2,8,22.
There is an evidence suggesting that
microvas-cular complications may develop and progress more rapidly in patients
with early onset type 2 DM, and that is due to an increased
tissue susceptibility to the damaging effects of hyperglycemia at a younger age23.
Similarly it has been reported that patients with DM diagnosed at < 45
years of age had a higher prevalence and more severe grades of diabetic
retinopathy than those diagnosed later, despite matched duration of DM and
glycemic control24. The younger age at onset of type 2 DM is an
independent risk factor for the development of diabetic retinopathy (the odds
ratio for diabetic retinopathy was 1.9, 1.1, and 1; when age at onset of DM was
< 45, 45 55 and > 55 years respectively)24.
Early detection of diabetic retinopathy in diabetic patients
should be planned in liaison with local general medical practioners. Arranging
screening programs for all ages especially between 40-60 years at the time of
diagnosis and thereafter annually.
CONCLUSION
Over
51% patients in our study had diabetic retinopathy on diagnosis with a mean age
of 30.5± 4.6 years. Majority of
the patients with type-2 DM (64%) had sight threatening proliferative diabetic
retinopathy with or without CSME on presentation ranging mostly in < 50
years age group. There is a higher prevalence of sight threatening DR (PDR or
CSME) in our patients with earlier presentation. Early onset of type-2 DM is
related to greater prevalence of sight threatening DR.
Authors Affiliation
Dr. Mohammad Memon
Department
of Ophthalmology, Liaquat University of Medical and Health Sciences,
Jamshoro/Hyderabad, Pakistan
Dr. Sajjad Ali Surhio
Department
of Ophthalmology, Liaquat University of Medical and Health Sciences, Jamshoro /
Hyderabad, Pakistan
Dr. Shahzad Memon
Department
of Ophthalmology, Liaquat University of Medical and Health Sciences, Jamshoro /
Hyderabad, Pakistan
Dr. Noor Bakht Nizamani
Department
of Ophthalmology, Liaquat University of Medical and Health Sciences, Jamshoro /
Hyderabad, Pakistan
Dr. Khalid Iqbal. Talpur
Department of Ophthalmology, Liaquat
University of Medical and Health Sciences, Jamshoro / Hyderabad, Pakistan
REFERENCES
1.
Shaw JE,
Sicree RA, Zimmet PZ. Global estimates of the prevalence of diabetes for 2010 and 2030.
Diabetes Res Clin Pract. 2010; 87: 4-14.
2.
Mahar
PS, Awan Z, Manzar N, Memon S. Prevalence of type-2 diabetes
mellitus and diabetic retinopathy: the Gaddap study. J Coll Physicians Surg Pak.
2010; 20: 52832.
3.
Shaya
FT, Aljawadi M. Diabetic retinopathy. Clin Ophthalmol 2007; 1: 25965.
4.
Shaikh
A, Shaikh F, Shaikh ZA, Ahmed J. Prevalence of Diabetic
Retinopathy and influence factors among newly diagnosed Diabetics in Rural and
Urban Areas of Pakistan: Data analysis from the Pakistan National Blindness
& Visual Impairment Survey 2003. Pak J Med Sci. 2008; 24: 7749.
5.
Chaudhary
GM. Retinopathy in diabetic patients. Pak J Med Res. 2005; 44: 82-7.
6.
Shah CA.
Diabetic retinopathy: A comprehensive review. Indian J Med Sci. 2008; 62: 500-19.
7.
Mohan V,
Sandeep S, Deepa R, Shah B, Varghese C. Epidemiology of type 2
diabetes: Indian scenario. Indian J Med Res. 2007; 125: 21730.
8.
Basit A,
Hydrie MZI, Hakeem R, Ahmedani MY, Masood Q. Frequency of chronic
complications of type 2 diabetes. J Coll Physicians Surg Pak. 2004; 14: 7983.
9.
Niazi
MK, Akram A, Naz MA, Awan S. Duration of Diabetes as a Significant
Factor for Retinopathy. Pak J Ophthalmol. 2010; 26: 182-6.
10.
AlMaskari
F, ElSadig M. Prevalence of diabetic retinopathy in the United Arab Emirates: a
cross sectional survey. BMC Ophthalmol. 2007; 7: 11.
11.
Agrawal
RP, Ranka M, Beniwal R, Gothwal SR, Jain GC, Kochar DK, et al.
Prevalence of Diabetic Retinopathy in Type 2 Diabetes in Relation to Risk
Factors: Hospital Based Study. Int J Diab Dev Ctries. 2003; 23: 16-9.
12.
Khandekar
R, Al Lawatii J, Mohammed AJ, Al Raisi A. Diabetic retinopathy in
Oman: a hospital based study. Br J Ophthalmol. 2003; 87: 1061-4.
13.
Kayani
H, Rehan N, Ullah N. Frequency of Retinopathy among diabetics admitted in a teaching
hospital of Lahore. J Ayub Med Coll Abottabad. 2003; 15: 53-6.
14.
Siddiqui
SJ, Shah SIA, Shaikh AQ, Depar MY, Abbassi SA. Study of
189 cases of diabetic retinopathy at CMC Larkana. Pak J Ophthalmol. 2007; 23: 92-6.
15.
Khan AJ. Age,
Sex and Duration Relationships and Prevalence of Diabetic Retinopathy in
Pakistani Population. Pak J Ophthalmol. 1990; 6: 6-8.
16.
Javadi
MA, Katibeh M, Rafati N, Dehghan MH, Zayeri F, Yaseri M et al.
Prevalence of diabetic retinopathy in Tehran province: a population based
study. BMC Ophthalmol. 2009; 9: 12.
17.
El
Haddad OA, Saad MK. Prevalence and risk factors for diabetic retinopathy among Omani
diabetics. Br J Ophthalmol. 1998; 82: 901-6.
18.
Bamashmus
MA, Gunaid AA, Khandekar RB. Diabetic retinopathy, visual impairment
and ocular status among patients with diabetes mellitus in Yemen: a
hospital-based study. Indian J Ophthalmol. 2009; 57: 293-8.
19.
Narendran
V, John RK, Raghuram A, Ravindran RD, Nirmalan PK, Thulasiraj RD. Diabetic
retinopathy among self reported diabetics in southern India: a population based
assessment. Br J Ophthalmol. 2002; 86: 1014-8.
20.
Ishaque
N, Rahman N. Prevention of significant Visual Loss in Diabetic Macular edema
by early Laser Photocoagulation. Pak J Ophthalmol. 1998; 14: 73-6.
21.
Aziz-ur-Rahman,
Aziz TM, Niazi JH. Use of Diode Laser in Diabetic Maculopathy. Pak J Ophthalmol.
2001; 17: 43-7.
22.
Iqbal F,
Naz R. Patterns of diabetes mellitus in Pakistan: An overview of the
problem. Pak J Med Res. 2005; 44: 59-64.
23.
Song SH,
Hardisty CA. Early onset type 2 diabetes mellitus: a harbinger for
complications in later years--clinical observation from a secondary care
cohort. QJM. 2009; 102: 799-806.
24.
Wong J,
Molyneaux L, Constantino M, Twigg SM, Yue DK. Timing
is everything: age of onset influences long-term retinopathy risk in type 2
diabetes, independent of traditional risk factors. Diabetes Care. 2008; 31: 1985-90.