Pediatric ocular diseases are of prime importance. Most of these
diseases are treatable up to a specific age and if left untreated may have a
disastrous effect on functional abilities of child. More specialized curative
services are required by the child population 1.It was reported that
there are 135 million people with true low vision in the world and among them 7
million are children (quantitatively a person is said to have true low vision
when he or she has visual acuity of 6/18 to light perception or visual field of
less than 10 degrees from point of fixation but uses or is potentially able to
use vision for planning and execution of a task)2. Approximately 1.3
million children in the world are blind, half of these cases are preventable
and treatable3.
About 60 – 80% children die within 2 years of onset of blindness either
due to underlying cause of blindness (general ailment or hereditary or systemic
disease) or due to lack of support for survival4.Various studies have
reported that pediatric ocular diseases and cause of visual loss in children
varies from place to place and greatly depends on socioeconomic conditions of
the area.5
In countries with low socioeconomic strata and inadequate
healthcare systems, malnutrition and infections form major part of the etiology;
while in industrialized countries common pediatric diseases are cataract,
glaucoma, retinopathy of prematurity, genetically transmitted diseases and
congenital abnormalities5.
In
addition childhood blindness has direct effect not only on the functional
abilities of child and education but also indirectly effects family and
community. This has drawn the attention of World health organization's Vision
2020 program which included “childhood blindness” as one of its major targets.
MATERIAL AND METHODS
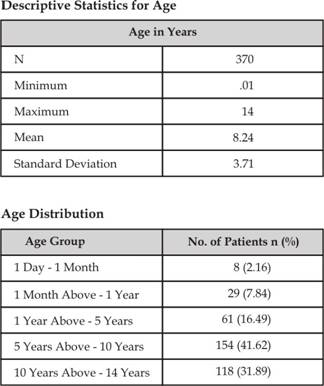
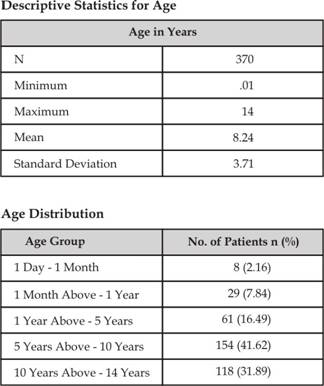
It was a hospital based descriptive cross sectional
study. The study was carried out at OPD of Spencer Eye Hospital Karachi from
March 2012 – May 2012. It included 370 patients of age from 1 day to 14 years
through non-probability consecutive sampling technique. Sample size was
calculated by using Open Epi sample size calculators for demographic studies.
Population size taken was 10,000, while keeping confidence interval 95%,
margin of error 5% and prevalence of conjunctivitis (P) 42%; the calculated
sample size was 370.
Informed consent was taken and anonymity and
confidentiality of the patient was maintained throughout the study.
A detailed
history was taken regarding the ocular disease and examination was carried out
in detail on slit lamp, direct and indirect fundoscopy was done where required.
Refraction was done and examination under anesthesia was done if required.
Diagnosis was established and recorded. Patients were managed accordingly. Data
analysis was done on SPSS programme version 14. Descriptive statistics were
used to calculate mean and standard deviation for age. Frequencies were
calculated for ocular diseases along with the percentages.
RESULTS
We studied 370 patients from March 2012 – May
2012. There were 220 (59.50%) male patients and 150 (40.50%) female patients.
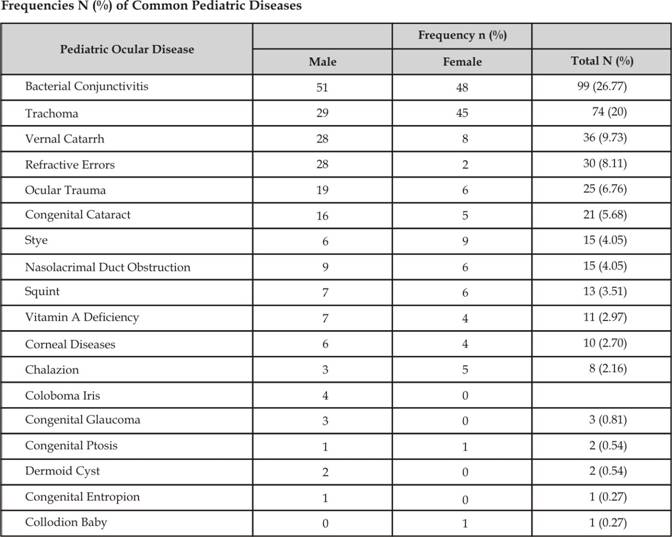
Bacterial
conjunctivitis was most frequently found ocular disease (26.77%) followed by
trachoma (20%) while vernal catarrh was present in 9.73% patients. Refractive
errors were present in 8.11% patients and ocular trauma in 6.76% patients.
Congenital cataract presented in 5.67% patients. Squint was found in 3.51%
patients. Presentation of corneal ulcer was in 2.7% patients. Congenital
diseases were not much prevalent for e.g. coloboma iris (1.08%) congenital
glaucoma (0.81%), congenital ptosis (0.8%), dermoid cyst (0.54%), cogenital
entropion (0.27%) and collodion baby (0.27%). It was observed that
conjunctivitis (m = 80, f = 93), stye (m = 6, f = 9) and chalazion (m = 3, f = 5)
are more prevalent among female children and vernal catarrh (m = 28, f = 8),
refractive errors (m = 28, f = 2) and ocular trauma (m = 19, f = 6) are more
prevalent among male children.
DISCUSSION
A male preponderance was seen 59.50% while female patients were 40.50%,
this finding was very similar to a study conducted at eye department Khyber
Teaching Hospital where male patients were 68.9% and female patients were
31.1%.6 This could be due to the fact that preference is given to
male children in poor society.
Most
frequently reported disease in our study was infectious conjunctivitis 26.77%
and trachoma 20%. A study conducted by Qureshi H M and et al reported7
prevalence of trachoma among children less than 10 years of age up to 48.98%.
This is higher than our study perhaps due to the fact that this study was
conducted in rural areas of upper Sindh where poverty and poor sanitation are
responsible for high prevalence of this disease. Stye and Chalazion were seen
in 4.05% and 2.16% children respectively. Spencer Eye hospital is located in an
old town of Lyari where
the hygienic conditions are not satisfactory and socioeconomic conditions
are also poor but not as worse as rural areas of Sindh. These factors may play
a significant role in high prevalence of infectious eye diseases in this area.
Poor sanitation, ignorance and poor hand washing
practices due to deficiency of water are additive factors. Prevalence of vernal
catarrh was 9.72% and a male preponderance was seen. Sethi S et al reported
35.6% prevalence of vernal catarrh with a male preponderance6. Their
results were noticeably different from ours perhaps due to geographical and dry
climatic conditions of that region.
Refractive errors were found in 8.11% patients.
Uncorrected refractive errors have a direct effect on learning capabilities of
the children and their education9. According to another study it was
reported that refractive errors are third largest cause of curable blindness in
Pakistan10.
In a study conducted by Sethi S6, prevalence of refractive
errors was 12.8% which is quite closer to the finding of our study. In another
study conducted in NWFP it was found that refractive errors were responsible
for 8% uniocular blindness and amblyopia11. Children who presented with ocular trauma were 6.76%.
Most of these cases presented with corneal cuts and prolapse of uveal tissue.
Lack of transportation was one of the major causes of delayed presentation of
these cases and poor prognosis. Sethi and et al reported in their study that
trauma accounted for half of peadiatric corneal disorders in their study6.
Another study reported that ocular trauma forms 8 – 14% of total injuries
suffered by children12.
Children are more prone to ocular injuries due to their inability to
avoid hazards13. Afghani T reported in his study on Causes of
Childhood Blindness that 6% of childhood blindness was due to postnatal causes
and major underlying pathology in his study was ocular trauma14.
Presentation of congenital cataract was 5.68%.More than
50% of these cases were due to congenital rubella and about 30% were familial
with a positive family history. No cause could be established in few
cases. Sethi S et al reported in their
study that lens disorders are responsible for 8.9% of the paediatric ocular
disorders quite similar to our study and among them bilateral congenital
cataract is the most common cause6. Another study by Sethi and Khan
reported 4.91% prevalence of bilateral congenital cataract15. Rahi
and Sripathi have reported that 20-30% of childhood blindness is due to
cataract. Majority cases of bilateral congenital cataract in developing
countries are due to congenital Rubella16.
Patients with nasolacrimal duct obstruction were 4.05%.
Sethi et al reported 5.07% of these cases in their study which is quite similar
to our study. 80 – 90% of these patients responded well to syringing and
probing. Presentation of children with squint was 3.51%. Majority of them had
esotropia. A study conducted in Nepal reported 1.6% prevalence of squint16
and a Tanzanian study reports 0.5% prevalence of squint17. Presence
of a well developed squint clinic may be helpful in early diagnosis and management
of strabismus as esotropia may have an amblyopic potential.
Vitamin A deficiency has a major contribution towards
preventable corneal blindness and there is a great variation in its prevalence
in same region as well as region to region. In our study ocular involvement due
to vitamin A deficiency was 2.97%.These children were severely malnourished.
Afghani T reported this prevalence up to 12%15. Another study
conducted at Lasbela Baloshistan reported the same 3.29%20 while the
prevalence reported from India was 26%16.
Presentation of children with corneal disorders was
2.70%. Greater presentation was of bacterial corneal ulcers. Many of them
presented as post measles corneal ulcers. Sethi and et al Reported 4.9% the
prevalence of corneal diseases16. They reported the same prevalence
in another study conducted at Khyber teaching hospital Peshawar6.
These findings are almost 50% greater than that of our study. In another survey
by Afghani T corneal diseases formed 12% of all the pediatric diseases14.
Most of these causes are responsible for preventable blindness.
Our study reported 0.81% cases of congenital glaucoma
which is quite similar to the study conducted at Khyber Teaching Hospital where
it was reported 0.99%6. While another study conducted, these cases
present so late that many children have become blind. Poverty, Ignorance,
Illiteracy and lack of transport facilities are responsible for such cases of
preventable blindness.
Prevalence of congenital ptosis was 0.54%. The study
showed 0.12% prevalence of congenital ptosis. Severe cases of ptosis require
early treatment as chances of development of amblyopia are greater in severely
drooped eyelid.
Congenital diseases were not much prevalent for e.g.
congenital glaucoma (0.81%), congenital ptosis (0.54%), dermoid cyst (0.54%),
cogenital entropion (0.27%) and collodion baby (0.27%). It was observed that
conjunctivitis, stye and chalazion are more prevalent among female children and
vernal catarrh, refractive errors and ocular trauma are more prevalent among
male children.
A very interesting entity was of collodion baby 0.27% who
presented to us on 2nd day of his life.
The term collodion baby is used for newborns in which all
the body surface is covered by thick skin sheets, so called “collodion membrane”. In almost all of the collodion membrane cases an autosomal recessive
ichthyosi form disease is implicated20. The eyelids and the lips may be everted and tethered
(ectropion and eclabion). In such cases loss of proper management can result
with keratitis due to xerophthalmia and eventually blindness21-24).
CONCLUSION
Paediatric ocular disorders are of utmost importance. Their early
diagnosis and prompt treatment is greatly helpful in reduction of preventable
causes of childhood blindness. Ignorance, illiteracy, poverty and lack of
transport facilities are mainly responsible for these situations. Such outcomes
directly affect the functional abilities of the child and his education and
indirectly his family and community. It should be the responsibility of electronic media to educate people
about the importance of various pediatric diseases.
Author’s Affiliation
Dr. Uzma
Fasih
Associate
Professor
Spencer
eye Hospital Unit 2
Karachi Medical & Dental College
Dr. Atiya
Rahman
Assistant
Professor
Spencer
eye Hospital Unit 2
Karachi Medical & Dental College
Dr. Arshad
Shaikh
Prof.r and
Head of Ophthalmology Department
Karachi Medical & Dental College
Dr. M. S.
Fahmi
Professor
and Incharge
Spencer
eye Hospital Unit 2
Karachi Medical & Dental College
Dr. M.
Rais
Senior Registrar
Spencer
eye Hospital Unit 2
Karachi Medical & Dental College
REFERENCES
1.
Qayyum Z, Khan AM. Causes of low vision among children and
adult patients presenting at low vision clinic of Mayo hospital, Lahore
Ophthalmology Pakistan. 2008; 1: 34-370
2.
Chaudhry M. Low Vision Aids Ist edition India Japee
Brothers; World Health Organization. Prevention of childhood blindness. Geneva
WHO. 1992; 2006: 63.
3.
Gilbert CE, Foster A, Negral AD, Thylefors B.
Childhood Blindness A
new form of recording visual loss in children Bull World Health Organ ization.
1993; 71: 485-9.
4.
Rahi J S, Sripathi S, Gilbert C E, Foster A. Childhood Blindness due to vitamin A
deficiency in India: regional variations Arch. Dis Child. 1995; 72: 330-3.
5.
Gilbert CE, Canvas R, Foster A. Causes of blindness and sever visual
impairment in children in Chile. Dev Med Cild Neurol. 1994; 36: 326-33.
6.
Sethi S, Sethi JM, Saeed N, Kundi KN. Pattern
of common eye diseases in children attending outpatient eye department Khyber
Teaching Hospital. Pak J Ophthalmol. 2008; 24: 166-70.
7.
Qureshi MH, Siddiqui JS, Pechuho AM, Shaikh
D, Shaikh AQ. Prevalence
of trachoma in upper Sindh. Pak J Ophthalmol. 2010; 26: 118-21.
8.
Garcia – ferrer FJ, Ivan R, Vaughn DG. General Ophthal-mology, Mc Graw Hill Lange Company
2008; 17: 103-14.
9.
Negral AD, Maul EP. Pokheral, Zhap Refractive error study in
children: Sampling and measurement methods for a multicountry survey. Am J
Ophthalmol. 2000; 129: 421-6.
10.
Durrani J., Blindness Statistics for Pakistan Pak J Ophthalmol. 1994;
10: 39-42.
11.
Khan MA, Gullab A, Khan MD. Prevalence of blindness and low vision in
North West Frontier Province of Pakistan. Pak J Ophthalmol. 1999; 15: 1-2.
12.
Scribano PV, Midelfart, Nance M, Reilly P. Peadiatric non powderFire arm injuries.
Outcomes in urban peaditrric setting. Peadiatrics 1997; 100: 5.
13.
Negral AD, Thlefors B. The global impact of eye injuries. Ophthalmic
Epidemiology. 1998; 5: 143-69.
14.
Afghani T. Causes of Childhood Blindness and severe Visual
impairment. Pak J Ophthalmol. 2000; 16: 4-26.
15.
Sethi S, Khan MD. Survey of Blind Schools in North West
Frontier province. Pak J Ophthalmol. 2001; 17: 90-6.
16.
Rahi JS, Sripathi S, Gilbert CE. The importance of perinatal factors in
childhood blindness in India. Developmental Medicine and Child Neurology. 1997;
39: 449-55.
17.
Nepal BP, Koirala S, Adhi KS. Ocular morbidity in school children in
Khatmandu. BR J Ophthalmol. 2003; 87: 531-4.
18.
Wener Susamme HW, David AR. Rebecca B et al. Prevalence of eye diseases
in primary school children in rural areas of Tanzania BR J Ophthalmol. 2000;
84: 1291-97.
19.
Khalil A, Lakho M, Jadoon Z. Pattern of Ocular Problem in school going
children of district Lasbela, Balochistan. Pak J Ophthalmol. 2012; 28: 200-5.
20.
Tüzün Y, İşçimen A, Pehlivan O. Collodion Baby J Turk Acad Dermatol. 2008;
2: 82201.
21.
Judge MR. Collodion baby and Harlequin ichthyosis. Harper J,
Oranje A, Prose N. Textbook 0f Pediatric Dermatology. Second edition. Malden, Blackwell
Publishing. 2006; 118-25.
22.
Shwayder T, Akland T. Neonatal skin barrier: structure, function
and disorders. Dermatol Therapy. 2005; 18: 87-103.
23.
Judge MR, McLean WHI, Munro CS. Disorders of keratinization. Burns T,
Breathnach S, Cox N, Griffiths C. Rook's Text book of Dermatology. 7th ed.
Malden, Blackwell Publishing. 2004; 34: 1-34.
24.
Fleckman P, Digovanna JJ. The Ichthyoses. Klaus W, Goldsmith LA, Katz
SI, Gilchrest BA, Paller AS, Leffell DJ. Fitzpatrick’s Dermatology In General
Medicine. 7th edition. New York, McGraw – Hill Medical. 2008; 401-24.