Childhood blindness is a priority of Vision 2020: the Right
to Sight, the global initiative to reduce the worlds burden of avoidable
blindness1,2. Globally
there are estimated 1.5 million blind children, almost three-quarters of them living
in developing countries3. The prevalence of blindness in
children in Pakistan is estimated to be about 10 per 10,000 children4.
Various studies across the globe show one third
to half of childhood blindness is either preventable or treatable 5.
Cataract is the leading treatable cause of childhood blindness in children6,7.
Worldwide
5 20% of the blindness in children is due to congenital cataract and the
global incidence of congenital cataracts has been reported to be 1 15/ 10,000
live births7. A hospital based study in Pakistan showed that 54.7%
of the children are visually handicapped and 23% of them are because of
congenital cataract8.
Congenital
cataract usually present as a whitish reflex called leukocoria in eye. The
morphology of cataract is important because it may indicate a likely etiology,
mode of inheritance and effects on vision9. Congenital cataract requires early detection and treatment to prevent
permanent visual impairment from amblyopia (lazy eye)10. Earlier cataract
surgery with adequate visual rehabilitation contributes a better visual outcome11.
Optimal surgical treatment of the pediatric cataract
requires a procedure that will provide a clear optical axis. The visual axis
may be obstructed by posterior capsule opacification, inflammatory membranes,
thickening and opacification of the hyaloid face, and proliferation of the lens
epithelial cells12. Leaving the posterior capsule intact in children
predisposes to an unacceptably high rate of capsule opacification13,14.
To reduce the rate of visual axis opacification in the post operative period
posterior continuous curvilinear capsulorhexis with anterior vitrectomy, has
become the gold standard in the treatment of congenital cataract15.
This procedure will give a clear visual axis with a reduce rate of visual axis
opacification and postoperative need of yag laser capsulotomy. Along with
posterior capsulotomy and anterior vitrectomy implantation of
posterior chamber intraocular lenses (PC IOL) in children is becoming more
common and better accepted procedure throughout the world16.
There are various postoperative
complications encountered in children after surgery. Increased reactivity of
uveal tissue in children causes formation of membranes, fibrinous reaction and
posterior synechie. It may results in pupillary block and cause raised intraocular
pressure postoperatively17.
The rationale of this study is
to determine the outcomes of congenital cataract surgery in a series of
patients in tertiary care hospital.
MATERIAL AND METHODS
A total
of 192 eyes of 120 patients aged 3 to 8 years with visually significant
congenital cataract (≥ 3mm diameter) treated and followed up at our
hospital between July 1st, 2011 and January 31st, 2013, were included in
this interventional study. The study was
performed at Layton Rehmatullah Benevolent Trust Eye Hospital Karachi. Informed
consent was taken from the guardians. Exclusion criteria were other congenital
anomalies like microphthalmia and microcornea, history of intrauterine
infections, traumatic cataract, congenital glaucoma, nystagmus, ptosis,
strabismus, retinal pathologies and fundal dystrophies, systemic disorders like
galactosemia, hyper and hypoglycemia and complicated surgeries. After detailed
history patients were examined thoroughly and relevant investigations were
done. Ophthalmic checkup including visual acuity, slit lamp examination of
anterior and posterior segment,
keratometery, B-scan ultrasonography and intra ocular
lens power calculation wherever possible
were done. Un-cooperative children were examined under general anesthesia
before surgery for keratometry and intraocular lens power calculation. Intra
ocular lens power was calculated by
using SRK II formula.
Pre operatively dilatation of pupil was done by using
cyclopentolate 1% and phenylepherine 2.5%. Under general anesthesia and
sterilized draping supero-temporal limbal incision of 3mm was made with surgical
knife no.3.2. A viscoelastic agent was injected to maintain the anterior
chamber depth and facilitates easy entry of instruments with less surgical
trauma during surgery. Anterior capsulorrhexis was done by a bent 26 gauge
needle or utrata forceps according to the elasticity of anterior capsule. Lens
matter aspiration was done by means of an irrigation-aspiration hand piece.
After aspiration of lens matter posterior chamber foldable acrylic intra ocular
lens was implanted in the bag on posterior capsule. Posterior capsulotomy and
anterior vitrectomy was performed. Incision was closed by one interrupted 10-0
monofilament nylon suture and an air bubble is injected so as to maintain
anterior chamber depth postoperatively.
One
drop of topical atropine 1% and an antibiotic was instilled and pad applied.
Dressing removed after 24 hrs. Systemic antibiotics were given for five days
after surgery. Topical antibiotics, steroids and cycloplegic were given in the
follow-up period for six weeks.
Patients
were followed on 1st post operative day and 1st post operative week
for early postoperative complications and then patients were followed after 1
month, 3 months and 6 months. Visual acuity was assessed using the Lea symbols
and ETDRS charts depending on the age, intelligence and cooperation of child.
Amblyopia therapy was given to those whose visual acuity was greater than Log MAR
0.5. The therapy was given according to the age and density of amblyopia.
Occlusion of normal eye with better visual acuity was done by means of a patch
applied to that eye. Hours of patching depends on the age of the child. These
patients were followed at one month interval to monitor the improvement of
vision. Final visual acuity was assessed at 6 months and considered to be good
if it ranged between Log MAR 0.0 to 0.5.
RESULTS
A total
of 192 eyes of 120 patients with visually significant congenital cataract were
included in this study. Out of 120 patients, 70 (58.3%) were males and 50 (41.6%)
were females. Regarding site of eye, 102 (53.1%) left and 90 (46.9%) right eyes
were involved.
Mild to
moderate anterior chamber inflammation (up to Grade +2 anterior chamber cells
and flare) was seen in 25 (13%) eyes on first postoperative day. Patients were
treated with topical prednisolone aceatate 1% and cyclopentolate 1% and were
closely followed. Anterior chamber inflammation was completely settled after 2
weeks. Severe anterior chamber inflammation (Grade +3 to +4 anterior chamber
cells and flare) with pupillary membrane was seen in 30 (15%) eyes on first
post operative day. They received topical and systemic steroids treatment for 2
weeks along with atropine 1% Inflammation
settled down in 20 (10%) children while 10 (5%) children underwent Yag laser
membranectomy. Surgical membranectomy was not required as children were
cooperative. They were repeatedly followed after one week and prolonged steroid
treatment was given for one month. Post- operative inflammation was well
controlled in both the age groups and there was no visually significant
complication after treatment.
Raised
intra ocular pressure was seen in 10 (5.2%) eyes at first post operative week.
Those patients were treated with topical anti glaucoma medications (beta
blockers) and followed after one week to check intra ocular pressure. Intra
ocular pressure was settled down after one week with topical medication and did
not rise within the follow up period.
Pupillary
deviation was seen in 8 (4.1%) eyes. This was due to trauma to iris at the time
of surgery. Intraocular lens (IOL) capture was observed in 4 (2%) eyes.
Decentration of intra ocular lens was seen in 9 (4.6%) eyes. Small upward
decentration was seen in these cases and none of the IOL decentrations was
visually significant or a true dislocation, and no eye required surgical
repositioning of the IOL.
Loose corneal scleral sutures
were seen in 4 (2%) patients. Those sutures were removed under sedation in
younger children and at slit lamp in older and cooperative children.
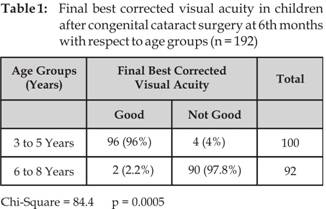
Final
outcome of best corrected visual acuity was assessed at the end of 6th month
after surgery. Mean BCVA at first month was 0.8 ± 0.15, at 3rd month
was 0.7 ± 0.19 and at 6th month was 0.5 ± 0.25 (Figure 1). Mean best
corrected visual acuity (range BCVA log Mar 0.0 to 0.5) was observed in 51%
(98/192) while not good (BCVA > 0.5) was observed in 49% (94/192) cases as
presented in figure 2. BCVA was significantly better in 3 to 5 years of age as
compared to 6 to 8 years of age (Table 1).
Follow-up
Duration![]()
Fig.
1: mean best corrected
visual acuity according to follow-up (n = 192)
BCVA
Fig. 2: Final best corrected visual acuity in children after congenital
cataract surgery at 6th months
There were no severe
complications encountered after surgery such as post operative endophthalmitis,
retinal detachment, glaucoma or significant postoperative inflammation with
lens deposits or synechias.
DISCUSSION
Congenital
cataract is the most common cause of visual impairment in children because of
sensory deprivation during the period of visual maturation 18. Its
etiology is multifactorial and among the various risk factors, most important
is the age of child. Management of the posterior capsule, aggressive amblyopia therapy, and
refractive management are major factors governing the ultimate visual outcomes
of congenital cataract surgery15. Many surgical procedures have been used to reduce the rate
of posterior capsular opacification in children. Posterior chamber intra
ocular lens implantation with posterior capsulotomy and anterior vitrectomy is
the most accepted surgical procedure in management of congenital cataracts16.
The age
at which anterior vitrectomy and posterior capsulotomy should be performed is
controversial. Many studies have different results. Basti et al performed primary posterior capsulotomy with
anterior vitrectomy in children younger than 8 years14. Dahan and
Salmenson recommended posterior capsulorhexis and anterior vitrectomy in
children younger than 8 years 19. Vasavada and Desai suggested that
anterior vitrectomy with posterior continuous curvilinear capsulorhexis was
desirable in children with congenital cataracts younger than 5 years20.
In our study we performed anterior vitrectomy and posterior capsulotomy in all
cases so as to minimize the rate of visual axis opacification and to achieve
early postoperative visual rehabilitation.
In our
study after treatment of postoperative complications and amblyopia therapy 51%
of eyes achieved good best corrected visual acuity (BCVA). It ranges from 0.0 to
0.5 Log MAR. Vision was not improved in 49% eyes despite proper management of
complications and aggressive amblyopia therapy. The results of good visual
acuity after congenital cataract surgery are variable. Kim et al reported
improved visual acuity in 51.7% of patients7. Lai et al showed
improvement in 50% of patients21. Magnusson et al reported 50% of
children achieved improvement in vision after surgery22.
In
follow-up period visual acuity was not improved during the 1st month
but in subsequent follow-ups most of the patients achieve good vision with mean
value of Log MAR 0.5. Magnusson et al also showed a mean value of Log MAR 0.5
at the end of followups22.
Improvement
in visual acuity after congenital cataract surgery was seen in patients who
presented in younger age. In younger age group of 3 - 5 years 96% of children
achieved good vision as compared to older age group of 6-8 years in which only
2% achieved good vision. In older age groups late intervention was the cause of
decreased vision because of form deprivation due to cataract during the
sensitive period of visual maturation. This showed that visual outcome
following cataract surgery depends on the age and earlier cataract surgery is
beneficial in achieving good vision11.
Moderate
anterior chamber inflammation was seen in 13% and severe inflammation was seen
in 15% of eyes. Keech et al reported 10% of eyes developed inflammation and
secondary membrane formation23. Zwaan et al reported 13% of eyes
developed fibrinous membranes after surgery24. Raised intra ocular
pressure was seen in 5% of eyes. Ondraaek and Lokaj reported raised introcular
pressure in 4.3% of cases25.
Pupillary deviation was seen in
4.1% of eyes. Ondraaek and Lokaj reported pupillary deviation in 3.8% of eyes25.
IOL capture was observed in 2% of eyes. Luo et al observed IOL capture in 2.6%
of patients26.
CONCLUSION
This study concludes that timing of the congenital
cataract surgery is the most important factor for visual prognosis.
Authors Affiliation
Dr. Kanwal Latif
Resident Medical Officer
LRBT Free Base Eye Hospital
Kornagi
2½ Karachi-74900
Dr. Munira Shakir
Consultant Ophthalmologist
LRBT Free Base Eye Hospital
Kornagi
2½ Karachi-74900
Dr. Shakir Zafar
Consultant Ophthalmologist
LRBT Free Base Eye Hospital
Kornagi
2½ Karachi-74900
Dr. Syed Fawad Rizvi
Chief Consultant Ophthalmologist
LRBT Free Base Eye Hospital
Kornagi
2½ Karachi-74900
Dr. Saliha Naz
Resident Medical Officer
LRBT Free Base Eye Hospital
Kornagi 2½ Karachi-74900
REFERENCES
1.
Gogate P, Gilbert C.
Blindness in children: a worldwide perspective.
Community Eye Health. 2007; 20: 32-33.
2.
Chak M, Wade A, Rahi JS.
British Congenital Cataract Interest group. Long-term visual acuity and its
predictors after surgery for congenital cataract: findings of the British
congenital cataract study. Invest Ophthalmol Vis
Sci. 2006; 47: 4262-9.
3.
Sethi S, Sethi MJ, Saeed N, Kundi NK. Pattern of common eye diseases in children attending outpatient
eye department Khyber Teaching Hospital. Pak J Ophthalmol. 2008; 24: 166-71.
4.
Mahdi Z, Munami S, Shaikh ZA, Awan H, Wahab S. Pattern of eye diseases in children at secondary level eye
department in Karachi. Pak J Ophthalmol. 2006; 22: 145-51.
5.
Gogate P, Gilbert C, Zin A.
Severe visual impairment and blindness in infants: causes and opportunities.
Middle East Afr J Ophthalmol. 2011; 18: 109-114.
6.
Chandna A, Gilbert C.
When your eye patient is a child. Community Eye Health. 2010; 23: 1-3.
7.
Kim KH, Ahn K, Chung ES, Chung TY. Clinical
outcomes of surgical techniques in congenital cataract. Korean J Ophthalmol.
2008; 22: 87-91.
8.
Butt IA, Jalisl M, Waseem S, Abdul Moqeet, Inam-ul-Haq M. Spectrum of congenital and developmental anomalies of eye. Al
Shifa J Ophthalmol. 2007; 3: 56-60.
9.
Amaya L, Taylor D, Russell Eggitt
I, Nischal KK, Lengyel D. The morphology and natural history of childhood cataracts. Surv
Ophthalmol. 2003; 48: 125-44.
10.
Sethi S, Sethi MJ, Hussain I, Kundi NK. Causes of amblyopia in children coming to
ophthalmology outpatient department, Khyber Teaching Hospital, Peshawar. J Pak
Med Assoc. 2008; 58: 125-8.
11.
Ye HH, Deng DM, Qian YY, Lin
Z, Chen WR. Long
term visual outcome of dense bilateral congenital cataract. Chin Med J (Engl). 2007; 120: 1494-7.
12.
Nishi O. Fibrinous membrane formation on the
posterior chamber lens during the early postoperative period. J Cataract Refract
Surg. 1988; 14: 73-7.
13.
BenEzra D, Cohen E. Posterior capsulectomy in pediatric
cataract surgery; the necessity of a choice. Ophthalmology. 1997; 104: 216874.
14.
Basti S, Ravishankar U, Gupta S. Results of a prospective evaluation
of three methods of management pediatric cataracts. Ophthalmology. 1996; 103: 713-20.
15.
Petric I, Lonθar VL. Surgical technique and
postoperative complications in pediatric cataract surgery: retrospective
analysis of 21 cases. Croatian Medical Journal.
2004; 45: 287-91.
16.
Astle WF, Alewenah O, Ingram AD, Paszuk A. Surgical outcomes of primary foldable
intraocular lens implantation in children: understanding posterior
opacification and the absence of glaucoma. J Cataract Refract Surg. 2009; 35: 1216-22.
17.
Kariman F, Ali Javadi M, Reza Jafarinasab M. Pediatric cataract surgery. Iran J Ophthalmic
Res. 2007; 2: 146-53.
18.
Kaul H, Riazuddin SA, Yasmeen A, Mohsin S, Khan
M, Nasir IA, et al. A new
locus for autosomal recessive congenital cataract identified in a Pakistani
family. Mol Vis. 2010; 16:240-5.
19.
Dahan E, Salmenson BD. Pseudophakia in children:
precautions, techniques, and feasibility. J Cataract Refract Surg. 1990; 16: 75-82.
20.
Vasavada A, Desai J. Primary posterior capsulorhexis with
and without anterior vitrectomy in congenital cataracts. J Cataract Refract
Surg. 1997; 23: 645-51.
21. Lai J, Yao K, Sun ZH,
Zhang Z, Yang YH. Long
term follow up of visual functions after pediatric cataract extraction and
intra ocular lens implantation. Zhonghua Yan Ke Za Zhi. 2005; 41: 200-4.
22.
Magnusson G, Abrahamsson M, Sjostrand J. Changes in visual acuity from 4 to 12 years of age in children
operated for bilateral congenital cataract. Br J Ophthalmol. 2002; 86: 1385-9.
23.
Keech RV, Tongue AC, Scott WE.
Complications after surgery for congenital and infantile cataract. Br J
Ophthalmol. 1989; 108: 136-41.
24.
Zwaan J, Mullaney PB, Awad A,
al-Mesfer S, Wheeler DT. Pediatric intraocular lens implantation. Surgical results and
complications in more than 300 patients. Ophthalmology. 1998; 105: 112-8.
25.
Ondraaek O, Lokaj M. Visual
outcome after congenital cataract surgery. Long term clinical results. Scripta
Medica (BRNO). 2003; 78: 95-102.
26.
Luo Y, Lu Y, Lu G, Wang M. Primary
posterior capsulorhexis with anterior vitrectomy in preventing posterior
capsule opacification in pediatric cataract microsurgery. Microsurgery. 2008; 28:
113-6.