Orbital
tumors may be primary, secondary, metastatic extension from adjacent tissues –
sinuses, lids, Eye ball or manifestation of leukaemia. Tumors may be benign or
malignant; in children 90% are benign (Cystic) and 10% malignant. Studies by
various authors have given variable incidence of different tumors, depending on
age, race, region and study period.
Lymphoid
tumors, inflammatory lesions (Pseudo-tumor muccoele) vascular and cystic lesion
(dermoid and epidermoid are most common1. There are conditions,
which mimic orbital tumors such as thyroid ophthalmopathy usual presentation is
axial proptosis, decreased vision, restriction of E.O.M, pain, inflammation and
cosmetic disfigurement. The initial clinical evaluation of patient with orbital
mass (lesion is frequently inclusive to arrive at corrective diagnosis clinical
examination, blood tests, X-Ray P.N.S and Rhinological examination, B-Scan
ultrasound, CT Scan and MRI are done. Biopsy remains gold standard;
ultrasonography is a good diagnostic tool especially in tumors of solid, cystic
variety and thyroid orbitopathy2.
Primary orbital tumors if not
treated on time and adequately cause morbidity and mortality by local extension
and systemic metastasis.
MATERIAL AND METHODS
This is
a retrospective study includes all cases confirmed by histology. We excluded
cases of thyroid ophthalmopathy, congenital bony anomalies, orbital varicose
veins, pseudo tumors who responded to retrobulbar and systemic steroids. The
cases where histopathological slides showed multi cellular and anaplastic cell
appearance and diagnosis was speculative were also excluded.
We
sought opinion of paediatrition, radiologist and clinical pathologist where
necessary biopsy was done in all cases. Blood tests, CT Scan, MRI were done in
selected cases to assess site, size, spread to surrounding structures and plan
surgical approach.
CT Scan and MRI helped
clinically and morpholo-gically to differentiate orbital infections from benign
and malignant tumor of epithelial and connective tissue origin. Tumor within
muscle cone or advanced tumors invading sinuses on anterior cranial fossa were
referred to ENT and Neuro Surgeon respectively.
RESULTS
Age of
study cases varied from 6 months to 80 years and gender wise male were 23 and
female 19 (Table 1). The most common tumors were Lymphoma, squa-mous cell
carcinoma and retinoblastoma comprising 6 of each (Table 2). While other tumors
included Fibro Sarcoma, Lacrimal
Gland Tumor, Socket Tumor, tuberculous granuloma, neurofibromatosis (3 each),
optic nerve meningioma, Dermoid Cyst, Lymphoid Hyperplasia of Lacrimal Gland (2
each) and Schwa-nnoma, Metastatic
Tumor, Porocarcinoma (1 each) (Table 2). In squamous cell carcinoma 04
cases were extension from limbus (Fig. 6) and 2 cases were direct spread from
lid (Fig 7).
Regarding
Fibrosarcoma, first case of two year old female child had grown to larger
dimensions just within three months time. It shows rapid and aggressive growth
in children1. In a second case of 24 year old male, it had grown
slowly and was well differentiated. In a third case 55 year old woman, it had
grown slowly over a period of 5 years and was painless (Fig 3). On attempted
exentration, it was massive growth which bled profusely and had eroded bony
walls of maxillary sinus, lateral wall of nose and roof of orbital fossa.
Patient died three weeks post-operatively due to concurrent infection. As
regards lacrimal gland tumor adenoid cyst carcinoma occurred in a 40 year old
female. This tumor had local infiltrative and metastatic potential. It responds
to radio therapy but is not radio curable1. Rest three tumors were one case epidermoid
carcinoma of lacrimal gland origin and two cases of lymphoid hyperplasia.
Table 1: The gender breakup of
cases
Table 2: The percentage of
different types of tumors

Fig. 1: Fibrsarcoma
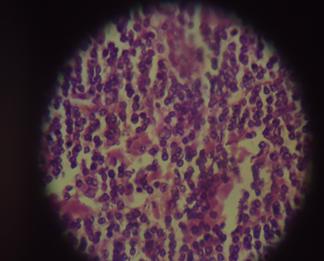
Fig. 2: Lymphoma
H.E Staining
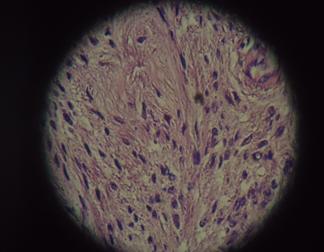
Fig. 3: Schwannoma
H.E Staining

Fig. 4: Meningioma
Optic Nerve
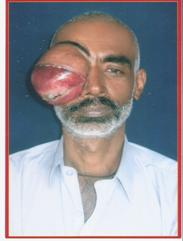
Fig. 5: Schawanoma

Fig. 6: Squamous
Cell Carcinoma
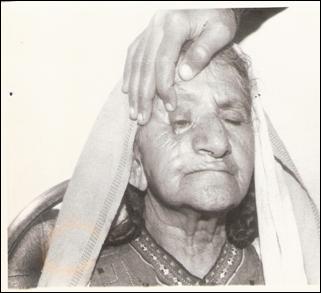
Fig. 7: Squamous
Cell Carcinoma Lid.
Two
cases of optic nerve menigioma were recorded. In both patients enucleation was
done: one 24 year old male had progressive proptosis, pain, lid oedema,
chemosis (Figure 4), for such growths similar description has been described
with age less than 10 years in literature11. Regarding nerve sheath
tumors, one schwannoma (Neurolimoma) and two Neurofibroma were recorded. Schwannoma
has been reported in two studies5,8 but without mention of
histological pattern and duration of onset.
Our
case (Fig 3) with 5 year duration is unique: bulky mass and easily enucleated
out without blood loss contrary to our expectations. Microscopically both
Antoni A-Spuidle cells in cords and whorls plus Antoni B-stellate cells with
mucoid stroma, coexisted in some cross sectional view1.
A nine
year old boy presented with painless proptosis of right eye of recent onset.
After clinical examination retrobulbar leukaemia deposits were suspected.
Peripheral blood film revealed blast cells. Patient was referred to
hematologist and was lost to follow up.
In 50
year old man with proptosis of few years duration exentration was done. A
diagnosis of poro carcinoma was made by Histopathologist after examination of
orbital contents. Incidentally secondary tumors with extension from adjacent
sinuses, nose brain were not encountered in our collection of 24 years
duration.
DISCUSSION
Incidence
of Lymphoma was higher as reported in recent studies3,4 followed by
squamous cell carcinoma and Retinoblastoma (Table 2). The two latter tumors are
listed equal to Lymphoma but are not primary tumors of orbit.
Out of
lymphomas, 04 cases were non Hodgkin’s (two large and two small) and 02 were
Hodgkin’s type. Our incidence was 13% but 7 – 20% has been reported in
literature and same reported by Jawaid in his study5. However in
Hodgkin’s type search for extra orbital involvement was not attempted. One case
of orbital Burkitt’s tumor (B-cell) arising from ethmoid sinus was reported in
a 5 year old boy6. In another report7 primary non
Hodgkin’s Lymphoma which involved left orbit and upper lid in a 4 year old
girl.
Editorial
by Awan8 quoted 24 year study (1962 – 1986) about 750 orbital tumors
although there was no mention of Burkitt’s tumor. He further stated that in
early nineties 200 – 300 cases were reported annually and that such tumors were
not recognized or misrecognized by the pathologists. Both Hodgkin’s and Non
Hodgkin’s Lymphoma have been reported in immuno deficiency syndrome9,10.
Out of
228 ophthalmic Lymphoma adenexal and ocular reported1 during 1980 – 2005
more than 50% were located in orbit with rapid rising incidence. Complete
remission or significant reduction of lymphoma lesions following antibiotic
therapy for Chlamydia psittaca infection – suggest its role in aetiology of
lymphoma11. Some authors also noted higher incidence of non
Hodgkin’s lymphoma in Asians than Europeans and blacks.
Relationship
between lymphoma and Chlamydia psittaci with regard to aetiology and response
to anti-bodies was previously reported by Ferri A et al in two separate papers
with different team of coauthors12,13.
Galieni
et al.14 reported fifteen patients with localized orbital lymphoma
and low grade mucosa associated lymphoid tumor (MALT) which were treated with
chemotherapy, radiotherapy and surgical excision with local relapse in three
but disease spread was never recorded.
Hodgkin’s
and Non Hodgkin’s classification depends on variable histological cellular
pattern and morphology picture13-15.
Non
Hodgkin’s lymphomas are classified into B and T cells, B cells are much more
common and consist of large B cells, small cells and marginal cells. Burkitt’s
tumor is composed of large B Cells. Biopsy is sent to molecular diagnostic laboratory
and following methods applied.
- Immuno histochemistry with surface
cell markers for B and T cells15.
- Florometry
Genetic
study (Chromosomal dependant) for definitive diagnosis and subtyping of
lymphoma16,17.
In our opinion, modern
diagnostic techniques mentioned were non existent/non-available to pathologists
of late 20th century, could explain lack of proper histological
diagnosis typing and subtyping.
CONCLUSION
The study revealed rising
incidence and prevalence of orbital lymphoma. Its incidence was even higher
than that of reported. Lymphoma tumor is localized, stationary, and occasionally
assuming large size. Modern laboratory techniques have revealed higher
incidence as reported in resent international study. Rising incidence and
occurrence of this tumor need to be confirmed by further studies in future.
Author’s
Affiliation
Prof. Faiz M. Halepota
Department of Ophthalmology
Muhammad Medical College,
Mirpurkhas, Sindh – Pakistan.
Prof. Khalid Iqbal Talpur
Chairman, Department of Ophthalmology
Liaquat University Eye Hospital Hyderabad,
Sindh – Pakistan
Dr. Mahesh Kumar Luhano
Clinical Pathologist, Department of ophthalmology
Liaquat University Eye Hospital
Hyderabad,
Sindh – Pakistan
Late Sher Muhammad Shaikh
Department of Pathology
Chandka Medical College, Larkana
Sindh – Pakistan
Dr. Abdul Rehman Siyal
Department of Pathology
Muhammad Medical College, Mirpurkhas
Sindh – Pakistan.
ACKNOWLEDGEMENTS
Authors extend thanks to Dr. Aijaz Ali Khooharo, Associate
Professor and Incharge Director, Advanced
Studies, Sindh Agriculture University Tandojam for his input in
interpretation of results.
REFERENCES
1.
Greer ocular pathology.
4. Blackwell Science; 1989. 241-57.
2.
Khalil M. Diagnostic role of
ultrasonography in orbital disorders. Ophthalmology Update 2010; 8: 17-21.
3.
Moslehi R, Devesa SS, Schairer C, Fraumeni JF Jr. Rapidly increasing incidence of ocular Non-Hodgkin Lymphoma. J
Natl Cancer Inst. 2006; 98: 936-9.
4.
SJO LD, Ralfkiaer E, Prause JU, et al. Increase
incidence of ophthalmic lymphoma in Denmark from 1980 to 2005. Invest
Ophthalmol Vis Sci. 2008; 49: 3283-8.
5.
Jawaid MA. Management of orbital
tumors. Pak J Ophthalmol. 2005;
21: 44-8.
6.
Muhammad Z, Khan D.
Orbital Burkitt’s Lymphoma, arising from Ethnoid sinus. Pak J Ophthalmol. 1991; 17: 87-9.
7.
Talpur KI. Orbital – Blephro
lymphoma. Pak J Ophthalmol. 2001;
17: 134-6.
8.
Awan K. (Editorial), Burkitt’s
lymphoma in Pakistan. Pak J Ophthalmol.
1991; 7: 85-90.
9.
Park KL, Gonis KM.
Hodgkin Lymphoma of orbit associated with acquired immunodeficiency syndrome.
Am J Ophthal. 1993; 116: 111-2.
10.
Antle CM, White VA, Horsman DE, Rootman J. Large cell orbital lymphoma in patient with acquired
immunodeficiency syndrome. Ophthalmology. 1990; 97: 1494-8.
11.
American Academy of
Ophthalmology 2006. Ophthalmic pathology; Intraocular tumors section 4. AAO,
San Francisco. 209-10.
12.
Ferreri AJ, Guidobomi M, Ponzoni M De Conciliis C,
Dell'Oro S,
Fleischhauer K,
Caggiari L,
Lettini AA,
Dal Cin E,
Ieri R,
Freschi M, Villa E,
Boiocchi M, Dolcetti R.
Evidence for association between Chlamydia
psittachi and ocular adenexal lymphomas. J Natl
Cancer Inst. 2004; 96: 586-94.
13.
Ferreri AJ Ponzoni M,
Guidoboni M,
De Conciliis C,
Resti AG,
Mazzi B,
Lettini AA,
Demeter J,
Dell'Oro S,
Doglioni C,
Villa E,
Boiocchi M,
Dolcetti R.
Regression of ocular adenexal lymphoma
after Chlamydia psittica eradicating antibiotic therapy. J Clin Oncol. 2005, 23: 5067-73.
14.
Galieni P, Polito E, Leccisotti A, Marotta G,
Lasi S,
Bigazzi C,
Bucalossi A,
Frezza G,
Lauria F.
Localized orbital lymphoma. Haematologica.
1997; 82: 436-9.
15.
Freedman AS, Nadler LM.
Immunologic markers in non-Hodgkin’s lymphoma. Hematol Oncol Clin North Am.
1991; 5: 871-89.
16.
Clack C Glaser SL,
Dorfman RF,
Bracci PM,
Eberle E,
Holly EA. Expert View of Non Hodgkin Lymphomas in population based cancer
registry reliability of diagnosis and subtype classifications cancer
epidermoid. Biomarkers Prev. 2004; 13: 138-43.
17.
Harris, N. Jaffe ES,
Stein H,
Banks PM,
Chan JK,
Cleary ML,
Delsol G,
De Wolf-Peeters C,
Falini B,
Gatter KC,
et al. A revised Euro-American
classification of Lymphoid neoplasms: a proposal from the International
Lymphoma Study Group. Blood. 1994; 84: 1361-92.