Scleral buckling
and cryopexy has been a time tested and valuable surgical technique for
repairing rhegmatogenous retinal detachments (RD)1. Although
there has been increasing trend towards Pars Plana Vitrectomy (PPV) and
internal tamponade as a primary treatment for rhegmato-genous RD, still, high
success rates of functional and anatomic outcomes can be achieved with scleral
buckling procedures2.
The steps in conventional scleral buckling include limbal
conjunctiva peritomy, recti muscle bridle sutures, localization and cryotherapy
to retinal breaks, application of scleral exoplants, subretinal fluid drainage
and injection of gas or air in vitreous cavity in case of superior breaks3.
It is important
that surgeon should be very efficient and comfortable with indirect ophthalmo-scopy
when performed intra-operatively for precise application of cryotherapy and
placement and
adjustment of position and height of scleral exoplants.
However, indirect
ophthalmoscopy presents the surgeon with a reverse and inverted image of fundus
which can cause significant difficulty in performing retinal procedures and
observing fundus at the same time.5 Also, indirect
ophthalmoscopy becomes less yielding in terms of details and accuracy in cases
of hazy media. Repeated use of indirect ophthalmoscopy also makes the procedure
inconvenient5.
Owing to advanced fundal viewing systems
and improved microincisional vitrectomy instruments, surgeons have recently
tried to evaluate the feasibility of viewing fundus using contact and
noncontact lens during scleral buckling procedures with excellent results.6
In this series, we have performed modified scleral buckling procedures
utilizing noncontact fundal viewing system and endoillumination; thus
alleviating the need of using indirect ophthalmoscope intra operatively.
MATERIAL AND
METHODS
This prospective
interventional study was conducted in Vitreoretinal section of Al Ehsan Welfare
Eye Hospital,
Limbal conjunctival
peritomy was performed with 2 radial relaxing incisions 180° apart avoiding the
quadrants where final placement of scleral exoplant was planned.After peritomy,
all 4 recti muscles were engaged with squint hooks and bridle sutures were
passed underneath them using 4 – 0 silk suture. After consulting the RD
diagrams of patient, a 23 G Autoseal PMS cannula (Oertli® Instruments AG,
Switzerland) (Figure 1) was introduced 3.5 mm away from limbus (4 mm in phakic
patients), using 1 step 23 G trocar (Oertli® Instruments AG, Switzerland).
Placement of cannula was 120° away from the meridian of retinal break (or a
location that afforded maximum globe maneuvering while keeping the distance
between cannula and break at least 3 clock hours). A self retaining custom
modified (Chandelier type) 23 G endoilluminator (Figure 2) was inserted in the
Autoseal cannula.
Next, fundus was viewed through the aid of
surgical microscope equipped with Oculus Stereoscopic Diagonal Inverter
(OCULUS® Surgical, Inc. FL, USA) and Oculus Binocular Indirect Ophthalmo
microscope (BIOM®) with Oculus noncontact wide field enhanced lens (120° field
of view). After adjusting the image inverter, position of retinal break was
accurately marked on sclera. While viewing retina in the same way, cryotherapy
burns were applied at marked site. Endoilluminator was then removed and
circumferential solid silicone tyre/radial silicone sponge was secured with
sclera using mattress sutures with 5-0 Ethibond. Endoilluminator was again
inserted in vitreous cavity and final position and height of scleral exoplant
was adjusted while viewing retina through BIOM®. Subretinal fluid was drained
when needed in conventional manner and fundus was evaluated with scleral
indentation and for adequate retinal perfusion while observing central retinal
artery patency. Endoilluminator was removed along with 23 G cannula and the
site was secured with 6-0 Vicryl suture when needed. Isovolumetric
concentration of SF6 gas was injected in vitreous cavity through pars plana
where indicated. The surgery was completed by closing conjunctiva with 6-0
Vicryl suture.
RESULTS
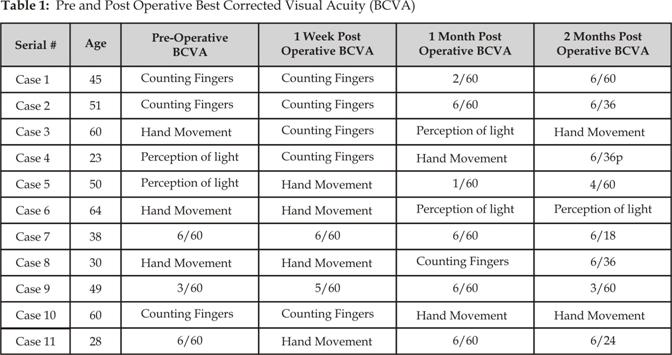
Out of 11 patients, 6 (54%) were male and 5
(46%) were females. 7 (63%) patients had RD in right eye and 4 (36%) had RD in
left eye. Range of age of patients was from 23 to 64 years with mean age of
45.3 years. 5 (45%) patients had solitary break whereas 6 (54%) patients had
more than one break. Distribution of breaks according to quadrants is shown in
Fig 3. 4 (36%) patients underwent radial silicone sponge where as 7 (64%)
patients under went solid silicone tyre with 360° silicone band. Anatomic
success was achieved in 82% of patients and functional success was achieved in
72% of patients as shown in Figure 4. BCVA of all patients is depicted in Table
1.
One patient had failed scleral bucking on first
post operative day with persistent inferior subretinal fluid.
Fig. 1. 23 G Auto Seal PMS Cannula with self sealing membrane.

Fig. 2. Self
retaining custom modified 23 G Endo Illuminator.
Fig. 3:
Quadrant wise Distribution of Retinal Breaks
Fig. 4: Anatomic and Functional outcome
after 2 month follow up
One patient had RD with grade C PVR 3 weeks
post surgery. Both patient had to undergo PPV and
silicone oil tamponade to reattach the retinas. One patient had deterioration
of BCVA despite retinal reattachment. Her reason for progressively declining
BCVA was extensive epimacular membrane. This patient lost to follow up after 2
months. 2 patients had minimal subretinal hemorrhage immediately after draining
subretinal fluid without any long term complications.
DISCUSSION
Helmholtz is
credited with invention of first ophthalmoscope in 1850 that could be
effectively used for viewing retina7 and accurate description
of retinal breaks was made possible after 2 years by Coccius8
and von Graefe9. Over the next century, various instruments
for viewing retina rose to horizon before Schepens10
introduced the first clinically effective binocular indirect ophthalmoscope in
1947; and indirect ophthalmoscope has changed little since Schepens classic
description.
The concept of
modern scleral buckling (post Jules Gonin era) started with Custodis11
when he became the first surgeon to perform scleral buckling using
episcleralexoplant (polyviol) in 1949. His methods of scleral buckling
underwent various advancements in terms of materials used for scleral exoplants
and in methods of retinopexy before Lincoff introduced cryopexy and silicone
exoplants; thus introducing the basis of modern scleral buckling12.
Thistechnique demands an efficient use of binocular indirect ophthalmoscope
while viewing a reverse and inverted fundus image. Also its use is considerably
inconvenient and time consuming when it comes to performing cryopexy while
viewing fundus at same time; thus demanding a considerable degree of expertise.5
Repeated surgical maneuvers needed while performing intra-operative indirect
ophthalmoscopy may also render the media hazy; thus compounding the problem of
accurate retinal break localization and its cryopexy.
Recently, surgeons have utilized various
instruments used in modern day PPV to assist them in conventional scleral
buckling to overcome the drawbacks mentioned above. First of many such reports
came from Kumar where he used endo light pipe to localize subretinal fluid
drainage site while performing scleral buckling in hazy ocular media.13
Nam5 recently reported a series of 12 cases where he
successfully reattached retinas through sclera buckling with the help of 25-G
Chandelier light (Alcon, Chandelier lighting system, Fort Worth. TX, USA) and wide – field contact lens (Mini Quad;
Volk, Mentor, OH).
He concluded that endoillumination systems are much easier to use while doing
scleral buckling when compared to conventional methods of viewing fundus intra
operatively.