True
exfoliation or capsular delamination1 refers to thickening and
splitting of superficial part the lens capsule from the deeper part with
extension into the anterior chamber2. Pathogenesis of this rare
condition is unclear, and causes include exposure to intense heat or infrared
rays, uveitis, cataract surgery or trauma2-7. Idiopathic7,8
true exfoliation of the lens has long been under reported.
Retinitis
pigmentosa (RP) 9 is the term used for a set of hereditary disorders
of variable presentation, involving the photoreceptors and retinal pigment
epithelium, resulting in progressive visual loss due to photoreceptor death,
night blindness, and constriction of visual fields.
True exfoliation has never been reported in
a patient with retinitis pigmentosa. Although, this combination could be a
complete chance occurrence, but we decided to report this unique case.
CASE REPORT
A 73
year old man presented to our outpatient department of Fauji Foundation
Hospital, Rawalpindi, with complaints of gradual, progressive decrease in
vision of the left eye for the past four months. He also gave a vague history
of having difficulties in night vision. He had undergone cataract surgery in
the right eye, one and a half year ago, and had no problems with it. Otherwise,
he had never had any eye problems. He did not have any co morbid systemic
illness. Family history was also negative for any ocular disease. He had never
worked in a glass factory and did not give a history of exposure to infrared
light or trauma.
On examination, best corrected distance vision
in the right eye was 6/6, and in the left eye 6/36. Slit lamp examination
revealed bilateral arcus senilis, bilateral mid-peripheral iris atrophy,
pseudophakia OD, and the left eye showed a diaphanous membrane arising from the
anterior capsule; attached on one end, folding of the lamella on itself, and
floating and undulating in the anterior chamber (Figures 1 5). The lens had
grade 3 nuclear sclerosis, and cortical cataract grade 2. The pupils dilated
fully on mydriasis, with no signs what so ever of pseudoexfoliation.
Intraocular pressures were 17 mm Hg OD and 18 mm Hg OS. Fundus examination
revealed normal discs bilaterally, with a CDR of 0.2, bilateral mid-peripheral
bony spicules of retinal pigment, beyond the arcades, retinal pigment
epithelial atrophy extending from the mid-periphery to the macular periphery,
with relative preservation on the maculae and a dull foveal reflex. The vessels
were attenuated (Figures 6 8). Gonioscopy was done which revealed grade IV
angles by Shaffer classification and prominent iris processes.

Fig. 1: Slit lamp photograph
showing the capsular delamination, with the rolled lamella projecting into the
anterior chamber.
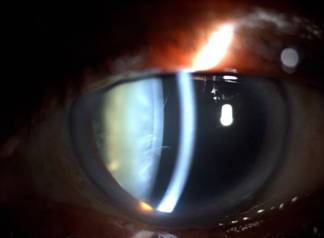
Fig. 2: The folded inferior
part of the true exfoliation

Fig. 3: Nuclear sclerosis Grade
3 and margins of the split layer

Fig. 4: Folded anterior capsule visible on nasal side

Fig. 5: Retroillumination
showing entire extent of the true exfoliation
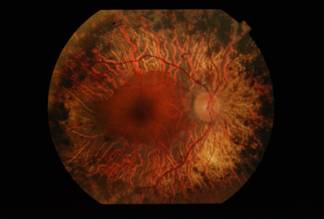
Fig. 6: Fundus photograph of
the right eye showing Classic Retinitis pigmentosa, with mid-peripheral bony
spicules, baring of RPE, vessel attenuation, and sparing of central macula.
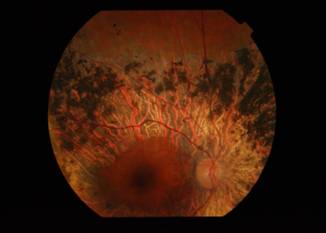
Fig. 7: A superior view of the
right fundus showing the mid-peripheral involvement
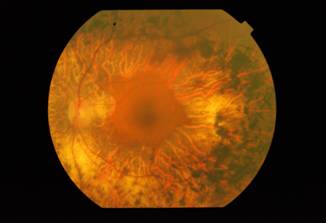
Fig. 8: Fundus photograph of
the left eye, showing retinitis pigmentosa, the view being hazy due to the
cataract
The
history of night blindness and associated signs in the fundus led to a clinical
diagnosis of classic RP, and since the maculae were spared, with good vision in
the right eye, and because often patients of RP give a vague history of night
blindness, and present to us when maculopathy occurs; no further investigation
was deemed necessary by us. The mid-peripheral iris atrophy can also occur in
elderly patients, and we consider it another chance occurrence, since there
were no signs of either pigment dispersion or pseudoexfoliation. He underwent
successful cataract surgery for the left eye, and best corrected distance vision
is 6/6 to date.
DISCUSSION
True
exfoliation is a so rare condition, that most textbooks do not explain it. It
was described for the first time10 in 1922 by Elschnig in
glassblowers, and later by Punder, who noticed floating anterior capsular folds
in a patient with a complicated cataract. The pathogenesis of this entity is
obscure. Usually, it is classically seen in people who have been exposed to
intense heat and infrared radiation over a long period, like glassblowers or
blast furnace operators. This may result in rupture of the lens capsule.
Recently, true exfoliation has been associated with trauma, ocular
inflammation, glaucoma, hypermetropia, senility, cataract surgery, and capsular
protein abnormalities.2-7,10,11 However; no one has ever described
an association with a pigmentary retinopathy.
Transmission
electron microscopy (TEM)11 has demonstrated loss of lens epithelial
cells along with abnormal fibrils which indicated age related degeneration as a
causative influence. Heat activated proteolysis, abnormalities in capsular
proteins and cellular abnormalities have been proposed as possible pathogenetic
mechanisms2.
True
exfoliation needs differentiation12 from the more common
pseudoexfoliation syndrome; the former being a splitting of the anterior
capsule with serrated or glistening, curled or scrolled margins, and the latter
being a dandruff like material deposited widely across the anterior segment,
and associated more frequently with an open angle glaucoma.
The
term retinitis pigmentosa13 is a misnomer due to the absence of
inflammation; and encompasses all retinal dystrophies with photoreceptor loss
and pigmentary retinal deposits. It has a prevalence of around 1:3000 to
1:5000. It is typically characterized by the classic triad of waxy disc pallor,
arteriolar attenuation, and bone spicule retinal pigment. Atypical RP has
many forms: pericentral, central, sectorial, sine pigmento, RP puntata
albescens, RP with exudative vasculopathy, and unilateral RP9, 13-15.
Diagnosis
is established by the presence of night blindness, fundus changes, progressive
visual field loss and diminished ERG a and b waves. Inheritance pattern of
RP may be autosomal dominant, autosomal recessive, X-linked or digenic. Ocular
associations of RP are many fold being; posterior sub-capsular cataract, open
angle glaucoma, myopia, keratoconus, optic disc drusen, vitreous cells, and
intermediate uveitis9, 13-15.
However our search of
literature has revealed that true exfoliation has never been reported in a
patient with RP, typical or atypical. Although, this may very well be a chance
occurrence, we believe that we are the first to report this instance.
Authors Affiliation
Dr. Sana Nadeem
Assistant Professor
Ophthalmology Department
Fauji Foundation Hospital / FUMC
Rawalpindi
Dr. Shahzad Waseem
Assistant Professor
Ophthalmology Department
Fauji Foundation Hospital / FUMC
Rawalpindi
Prof. Dr. B. A. Naeem
Professor and Head, Ophthalmology Department
Ophthalmology Department
Fauji Foundation Hospital / FUMC
Rawalpindi
Dr. Rabeea Tahira
Ophthalmology Department
Fauji Foundation Hospital / FUMC
Rawalpindi
REFERENCES
1.
Brodrick JD, Tate GW Jr.
Capsular delamination (true exfoliation) of the lens. Report of a case. Arch
Ophthalmol. 1979 Sep; 97 (9): 1693-8.
2.
Karp CL, Fazio JR, Culbertson WW, Green WR. True exfoliation of the lens capsule. Arch Ophthalmol. 1999; 117:
1078-80.
3.
Yamamoto N, Miyagawa A. True
exfoliation of the lens capsule following uveitis. Graefes Arch Clin Exp
Ophthalmol. 2000; 238: 1009-10.
4.
Cashwell LF Jr, Holleman IL, Weaver RG, van Rens GH. Idiopathic true exfoliation of the lens capsule. Ophthalmology.
1989; 96: 348-51.
5.
Tayyab A, Dukht U, Farooq S, Jaffar S. Spontaneous idiopathic true exfoliation of the anterior lens
capsule during capsulorhexis. J Pak Med Assoc. 2012; 62: 282-4.
6.
Oharazawa H, Suzuki H, Matsui H, Shiwa T, Takahashi H, Ohara K. Two cases of true exfoliation of the lens capsule after cataract
surgery. J Nippon Med Sch. 2007; 74: 55-60.
7.
Anderson IL, van Bockxmeer FM.
True exfoliation of the lens capsule. A clinicopathological report. Aust N Z J
Ophthalmol. 1895; 13: 343-7.
8.
Majima K, Kousaka M, Kanbera Y.
A case of true exfoliation. Ophthalmologica. 1996; 210: 341-3.
9.
Yanoff M, Duker JS.
Ophthalmology. Third Edition. Mosby: Elsevier. 2009; 550-9.
10.
Shentu XC, Zhu YN, Gao YH, Zhao SJ, Tang YL. Electron microscopic investigation of anterior lens capsule in an
individual with true exfoliation. Int J Ophthalmol. 2013; 6: 553-6.
11.
Riffle J. Floating anterior lens
capsule: an unusual case of true exfoliation. Digit J Ophthalmol. 2010; 16:
17-9.
12.
Theobold GD. Pseudoexfoliation of
the lens capsule: Relation to true exfoliation of the lens capsule as reported
in the literature and role in the production of glaucoma capsul-ocuticulare. Am
J Ophthalmol. 1954; 37: 1-12.
13.
Hamel C. Retinitis pigmentosa.
Orphanet J Rare Dis. 2006; 1: 40.
14.
Kanski JJ, Bowling B.
Clinical Ophthalmology: A systematic approach. Seventh Edition. Elsevier. 2011;
651-5.
15.
Regillo C, Chang TS, Johnson MW, Kaiser PK, Scott IU, Spaide R,
Griggs PB. American Academy of
Ophthalmology. Basic and Clinical Science Course. Section 12: Retina and
Vitreous. 2004; 207-11.