In
recent years, advances in cataract surgery have led to greater levels of
refractive precision, faster visual rehabilitation, improved comfort and safety.
Refinements in phacoemulsification techniques and intraocular lens (IOL)
technology deserve much of the credit for these advances, but innovations in
anesthesia, especially topical anesthesia, have also played an important role
in improving outcomes and visual recovery1. Peribulbar
injection of anesthetic agent has been used for cataract surgery for more than
a century, but it was associated with a high risk of injury to the orbital
contents. For the last two decades a number of modifications have been devised
to reduce the risks of injury to intra-orbital structures during administration
of peribulbar injection2. In 1884 Koller for the first time used
cocaine for Topical anesthesia3. After about a century Fichman
success-fully introduced a new method of injecting a local anesthetic agent for
cataract surgery which resulted in high patient satisfaction and faster visual
recovery4. Topical anesthesia increased from
8% in 1995 to 63% in 1998 for high volume cataract surgeries5.
A
number of studies have been conducted to assess patient’s satisfaction with
topical versus peribulbar anesthesia but these studies have conflicting results6,7.
Our
study assesses level of patient satisfaction in individuals who had bilateral
phacoemulcification with topical anesthesia in one eye and peribulbar block in
the other eye.
MATERIAL AND METHODS
The study was conducted in Combined Military Hospital Multan from
November 2012 to July 2013. 50 patients, 17 (34%) females, 33 (66%) males with
the ages between 59 to 74 years (mean age 66.5 years) having bilateral cataract
was included in this study. One eye was operated under topical anesthesia and
the other eye of the same patient with peribulbar block (50 eyes operated under
topical anesthesia and 50 eyes under peribulbar block). Eyes were randomly
selected for topical or peribulbar anesthesia. Uncooperative patients,
patients with allergy to lidocaine, poor pupillary dilatation (less than 3 mm),
anterior segment pathology, anxiety, dementia, deafness, nuclear sclerosis
grade 4 and ocular movement disorders were excluded from the study. During
their visit to the ophthalmology department, patients were informed about the
details of study well before the procedure. Consent was obtained from patients
and relatives for possible topical or peribulbar anesthesia, according to the
policy of our ethical committee.
Patient’s level of pain and discomfort was judged by the same
anesthesiologist in all cases to reduce bias.
All our
patients were day care cases. All surgical procedures were
performed by the same surgeon. Since all patients had to undergo bilateral
surgery the gap between bilateral surgeries was 30 days. Stabilization of the
globe was achieved by reducing the operating microscope light to the minimum
and asking the patient to look to the operating microscope light8.
Surgeon had continuous verbal communication with the patient and patient was
informed before performing certain steps like instillation of drops, making
incision, inserting phaco probe and implantation of intraocular lens.
Standardized 3 steps clear corneal incision was made using 2.8mm keratome,
supero-temporal for right eye and supero-nasal for left eye. One side port
paracentesis, was performed on left side of the main port. Viscoelastic
injection, continuous curvilinear capsulorhexis, hydro-dissection, hydro
delineation, phacoemulsification, aspiration of the residual cortical lens
matter, and implantation of foldable intra ocular lens in the bag was performed9.
At the end of surgery viscoelastic substance was removed, pupil was constricted
with intra-cameral 0.01% carbachol (Miochol)10, intra cameral 0.1 ml
0.5% Moxifloxacin eye drops was given in all cases. Wound margins were
hydrated, the self-sealing wound was checked for leakage by gentle compression
with a sponge. Postoperative treatments were similar in both groups;
Antibiotics and steroids combination eye drops were used
at 6 hourly interval slowly tapered off.
Anesthesia
(topical and peribulbar) was administered by the same anesthesiologist who also
recorded temperature, heart rate, blood pressure, chest auscultation, and blood
sugar level on anesthesia sheet. No patients received any oral sedation before
injection or operation. Patients used their routine drugs for treatment if any.
On the table, patients were connected to monitors for recording blood pressure,
ECG, respiratory rate and nasal / oral catheter for continuous supply of oxygen
at a rate of 3 – 5 liter per minute. In addition, 22 gauge intra venous cannula
was also inserted for any emergency.
Patients
in the peribulbar anesthesia group received one injection each, 4 ml mixed
solution of 0.5% bupivacaine hydrochloride (1.5 ml) and 2% lidocaine (2.5 ml)
into the lower peribulbar space of the eye9. Manual ocular
compression for 10 minutes was given to facilitate drug absorption. For all
patients the quality of peribulbar block was
assessed after 10 minutes which is the maximum fixation time for the local
anesthetic solution10. Block was considered acceptable if there was
no movement or slight flicker. Prior to the surgery, the surgeon also
assessed the effectiveness of block by eye
movements in four directions of gaze.
Eleven doses (approximately 40 μl per dose) of
proparacaine hydrochloride 0.5% were used in total (two drops on the cornea,
and one each in the superior and inferior conjunctival cul de sac) 15 and 10
min before surgery. Five minutes before surgery 2 more drops were instilled on
the cornea. One drop was instilled on the cornea before eye was padded. The
pain during surgery was controlled with additional 2 doses of 0.5% proparacaine
drops if required.
Pain was scored using visual analogue scale. Each
patient was shown a visual analogue scale with numerical and descriptive
ratings from 0 (no pain), 1 – 2 (slight stinging), 3 – 4 (mild pain), 5 – 8
(moderate pain) and 9 – 10 (severe pain). Patients were briefed about the use
of this pain scale to rate the level of pain felt Pre-operatively (during
administration of anesthesia topical / peribulbar), intra-operatively
i.e. phacoemulcification with intra ocular lens implantation (immediately after
surgery) and 4 hours post operatively. Discomfort
and feeling of pressure in the eye during administration of injection, during
surgery and 4 hours post operatively were assessed as No = 0 or Yes = 1. Patients who were unable to read the printed scale
were helped by the same colleague anesthesiologist who also performed the pain
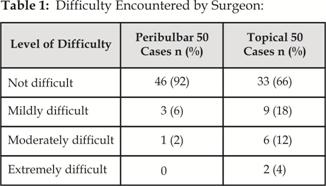
score recording in all the patients. The difficulties encoun-tered by the
surgeon during the surgeries were also graded as not difficult (grade 0),
slightly difficult (Patient uneasy = grade 1), moderately difficult (Patient
repeatedly squeeze eyes = grade 2) and extremely difficult requiring additional
analgesia (Unbearable pain = grade 3). Operating surgeon also completed the
form immediately after surgery.
Chi‑square test was used for categorical data. Numerical data
was analyzed using unpaired two tailed t‑test. Nominal data and proportions
were compared with Chi-squared analysis. A p < 0.05 was considered statistically
significant.
RESULTS
Fifty patients with bilateral cataract (100 eyes) were
included in the study. 50 eyes were operated with peribulbar block and 50 eyes
with topical anesthesia. During administration of anesthesia feeling of pain (p= 0.003), discomfort (p = 0.001) and feeling of pressure (p = 0.00) were significantly lower with
topical anesthesia as compared to peribulbar block (Fig 1 – 3). Intra operative
pain (p = 0.020), discomfort (p = 0.010) and feeling of pressure (p = 0.005) were higher in the topical
anesthesia group as compared to peribulbar block. Fig 1-3. Four hours post operatively pain (p = 0.000), discomfort (p
= 0.000) and feeling of pressure (p =
0.000) was significantly lower in peribulbar group than topical group. Fig 1-3.
Pain with Topical Anesthesia
y-axis no of patients x-axis pain
scale
Fig. 1a: Pain
Score during topical anesthesia:
Pain with peribulbar block
y-axis no of patients x-axis pain
scale
Fig. 1b: Pain Score with Peribulbar block:
Feeling of Discomfort
Fig. 2: Feeling of Discomfort:
Feeling of Pressure
Fig. 3: Feeling of Pressure:
DISCUSSION
Our study reveals that patients were more anxious, felt
more pain and discomfort in the eye that was operated under topical anesthesia,
however patients were more satisfied and calm during surgery with the other eye
that had phacoemulcification under peribulbar block. Our results were similar
to that of Boezaart et al11 who reported that patient who have never
experienced needle block may be satisfied with topical anesthesia while those
who have experienced both techniques preferred the peribulbar injection. Roman et
al22 also reported that the level of satisfaction of patient
undergoing cataract surgery with peribulbar block is much higher than topical
anesthesia.
In our study feeling of pain, discomfort and pressure
were higher with topical anesthesia. In contrast, surgery under peribulbar
anesthesia was painless despite the fact that patients felt comparatively more
pain, discomfort and pressure during the administration of injection. Others
have found no difference in pain perception when comparing topical with
peribulbar or retro-bulbar anesthesia12.
Fukasaku and Marror13, comparing topical
and peribulbar anesthesia, also reported more intraoperative pain in patients
receiving topical anesthesia for cataract surgery.
In recent years, topical anesthesia for cataract
surgery has gained popularity as safe and atraumatic technique14,15.
However, conflicting results have
been presented regarding pain, anxiety, patient discomfort and patient
satisfaction postoperatively with Topical anesthesia16.
The benefits of topical anesthesia over peribulbar or
retro-bulbar anesthesia are: no risks of the needle techniques, the analgesia
is immediate, no rise in intraocular pressure16, no need for globe
compression and no preoperative sedation.
Different methods have been tried to improve the pain
scores i.e. reduce pain in topical anesthesia. Lignocaine gel, instead of drops
gives low pain score due to prolonged contact time and better penetration17.
Although many surgeons used intra-cameral anesthetic along
with topical anesthesia, however no significant benefit is documented18.
The lack of akinesia is another drawback of the
topical anesthesia. Some surgeons find it difficult to work without akinesia;
however, as reported by many authors19 lack of akinesia does not
cause intra-operative difficulties to experienced surgeons.
A study conducted by Maclean H, Burton T
in 1997 revealed that most patients who received topical anesthesia do not feel
major pain, similar to patients who underwent surgery with peribulbar or
retrobulbar anesthesia,21 however, other studies have documented
that patients under topical anesthesia alone were more likely to experience
discomfort during manipulation of iris and zonular stretching21.
Roman et al have
reported that there is increased surgical difficulty with and a distinct
learning curve for topical anesthesia22. Jenkins et al
revealed that once the patient is cured there could be a bias from satisfaction
score23, however in our study this bias was minimized by the fact
that anesthesia (topical and peribulbar) was administered by and response of
all patients was recorded by the same anesthesiologist.
Patient satisfaction is one of the important healthcare
outcome measures. Results from several studies have shown that there is higher
patient satisfaction if postoperative pain is well controlled24. Despite
of pain and discomfort during administration of injection, both patients and
surgeons are more satisfied with the peribulbar block for cataract surgery due
to overall comfort.
CONCLUSION
Peribulbar anesthesia provides significantly better
patient satisfaction as compared to topical anesthesia during cataract surgery.
From surgeon’s perspective operating conditions with the peribulbar block is
also superior then topical anesthesia. Topical anesthesia is a safe
and an effective alternative to peribulbar anesthesia in cataract surgery.
However for effective and patient friendly topical anesthesia surgical
training, selection of cases, good preparation and education of patient,
measures to further minimize pain and discomfort are required.
Author’s Affiliation
Lt. Col. Dr. Zulfiqar-ud-Din Syed
Classified Ophthalmologist
Combined Military Hospital
Multan
Lt. Col. Dr. Tariq Mehmood Malik
Classified Anesthesiologist
Combined Military Hospital
Multan
Col. Dr. Aamir Mehmood Malak
Classified Anesthesiologist
Combined Military Hospital
Multan
Col. Dr. Dilshad Alam Khan
Classified Ophthalmologist
Combined Military Hospital
Multan
Maj. Dr. Umar Ejaz
Classified Ophthalmologist
Combined Military Hospital
Multan
Maj.
Dr. Arsalan Farooq
Trainee
Ophthalmology
Combined
Military Hospital
Multan
REFERENCES
1.
Colvard
DM, Kandavel R. Achieving excellence in cataract surgery; A step by step
approach; springer; 2009.
2.
Hamilton
RC. Brain stem anesthesia as a complication of regional anesthesia
for ophthalmic surgery. Can J Ophthalmol. 1993; 27; 323-5.
3.
Fichman
RA. Topical eye drops replace injection for anesthesia. Ocular Surgery
News. 1992; 1; 20-21.
4.
Konstantos
A. Anticoagulation and cataract surgery: A review of current
literature. Anaesth Intensive Care, 2001; 29; 11-8.
5.
Leaming
DV. Practice styles and preferences
of ASCRS members: 1998 survey. J Cataract Refract Surg. 1999; 25: 851-9.
6.
Said K, Hassan M, Qahtani FA. A comparative study of topical versus peribulbar
anesthesia in phacoemulsification and implantation of foldable intraocular lens
in cataract surgery. IJOVS. 2003; 2: available online only.
7.
Gangolf G, Jost BJ. Topical versus peribulbar anesthesia for cataract
surgery. Acta Ophthalmol Scand. 2003; 81: 596‑9.
8.
Salahuddin A. Cataract surgery: is it time to convert to topical anesthesia. Pak J Ophthalmol. 2008;
24; 2; 62-7.
9.
Crandall
AS. Zabriskie Inj of lidocaine intraocular increase patient
cooperative Ophthalmology. 1999, 106: 60.
10.
Gills
JP, Williams DL. Advantage of Marcain for Topical anesthesia. Journal of Cataract
and Ref. Surg. 1993; 819.
11.
Boezaart A, Berry R, Nell M. Topical anesthesia versus retro bulbar block for
cataract surgery: The patients’ perspective. J ClinAnesth. 2000; 12: 58‑60.
12.
Nauman A, Zahoor A, Saeed A M, Saba J, Waleed R. satisfaction level with Topical vs peribulbar
anesthesia experienced by same patient for phacoemulcification: Saudi J
Anesthesia. 2012; 6, 363-6.
13.
Fukasaku
H, Marror JA. Pinpoint anesthesia: a new approach to local ocular
anaesthesia. J Cataract Refract Surg. 1994; 20: 468-71.
14.
Jolliffe
DM, Abdel-Khalek MN, Norton AC. A comparison of topical
anesthesia and retrobulbar block for cataract surgery. Eye. 1997; 11, 858–62.
15.
Kershner
RM. Topical anesthesia for small incision self-sealing
cataract surgery. A prospective evaluation of the first 100 patients. J
Cataract Refract Surg. 1993; 19: 290-2.
16.
Jacobi
PC, Dietlein TS, Jacobi FK. A
comparative study of topical vs retrobulbar anesthesia in complicated cataract
surgery. Arch Ophthalmology. 2000; 118: 1037-43.
17.
Grabow
HB. Topical anesthesia for cataract surgery. Eur J Implant
Refract Surg. 1993; 5: 20-4.
18.
Bardocci
A, Lofoco G, Perdicaro S. Lidocaine
2% gel versus lidocaine 4% unpreserved drops for topical anesthesia in cataract
surgery. Ophthalmology. 2003; 110: 144-9.
19.
Gillow
T, Scotcher SM, Deutsch J. Efficacy
of supplementary intra-cameral lidocaine in routine phacoemulsification under
topical anesthesia. Ophthalmology. 1999; 106: 2173-7.
20.
Tsuneoka
H, Ohki K, Taniuchi O. Tenon's capsule anesthesia for cataract surgery with
IOL implantation. Eur J Implant Ref Surg. 1993; 5: 29-34.
21.
Maclean H, Burton T, Murray A. Patient comfort during cataract surgery with
modified topical and peribulbar anesthesia. J Cataract Refract Surg. 1997; 23:
277-83.
22.
Roman SJ, Auclin FX, Ullern MM. Topical versus peribulbar anesthesia in cataract
surgery. J Cataract Refract Surg. 1996; 22: 1121‑4.
23.
Jenkins K, Grady D, Wong J, Correa R, Armanious S,
Chung F. Post‑operative recovery: Day surgery patients’
preferences. Br J Anesthesia. 2001; 86: 272‑4.
24.
Seng TH,
Chen FK. A randomized clinical trial of combined topicalintra-cameral
anesthesia in cataract surgery. Ophthalmology 1998; 105: 2007‑11.