The word audit is
“a mean of quality control for medical practice by which the profession shall
regulate its activities with the intention of improving
overall patient care”1. An audit of clinical practice is the
analysis of the data either prospectively or retrospectively to determine both
quantitatively and qualitatively of the work load of an institution or
individual department. It includes numbers of admissions, patients’
demographics, various compli-cations and mortality2.
Previously
published literatures have shown that traumatic ocular injury was more common
in males3.They have also reported that open globe injury
was the most prevalent ocular emergency.
It has been found that younger workers (25 – 44) are more susceptible to
severe trauma4. It has been further reported that in India and other
developing countries corneal abrasion in agriculture-worker is a major risk
factor for causation of microbial keratitis5.
Ocular emergency cases are of
varied nature, from accidental foreign body injury to severe sight threatening
perforation of globe. In – spite of significant prevalence of ocular emergency in Burdwan
region no recent data is available. A five year retrospective clinical audit
from January 2008 to December 2012 is presented in this study to evaluate the
patients attending in the emergency department for ocular emergency services.
The aim of this audit is to determine the prevalence and causes of emergency
ocular problems in a medical college and hospital in rural setup.
MATERIAL
AND METHODS
A comprehensive
observational retrospective audit was done in the department of ophthalmology
Burdwan Medical College from January 2008 – December 2012.
The data was
collected from emergency inpatients registers, indoor admission registers, out
Patients registers and minor operation theater registers of the department of
ophthalmology. Data on patient age, gender, occupation, date of admission,
etiology of disease / trauma if any, presenting complains, and the treatment
offered to them were analyzed.
From the above database, patients were
classified into traumatic and non-traumatic ocular emergencies. Age and sex
distribution was studied among both the groups. According to the nature of
trauma the traumatic emergencies were further classified into: extra-ocular
foreign body induced injuries, open globe injuries and closed globe injuries.
Non traumatic ocular emergencies were further classified according to the
nature of the disease. Among the non traumatic group, corneal ulcers were
further sub-classified according to etiological agent.
RESULTS
Between January 2008 – December 2012, the Department of
Ophthalmology, Burdwan Medical College provided general and specialized
emergency services to 5,674 patients in total. Therefore on average 1,135
patients per year and about 3.15 patients/day attended the emergency Department
of Ophthalmology of Burdwan Medical College and Hospital.
Total 5,674 patients were seen /
admitted in the Ophthalmology emergency. Among them male and female were 3,764
and 1,910 respectively. Male: Female ratio was 1.97:1. The youngest patient in
this audit was 6 months old and the eldest was 90 years and the peak age group
was 2nd and 3rd decades of life. Traumatic ocular emergency cases
were 4071 (71.75%) and non-traumatic cases were 1603 (28.25%). The most common
traumatic ocular emergency was extra-ocular foreign body 1848 (45.40%) followed
by open globe injury 976 (23.97%). In traumatic ocular emergency male and
female were 3,044 (74.77%) and 1,027 (25.22%) respectively. Among extra-ocular
foreign body, the most common site of foreign body lodgment was cornea 1,280 (76%)
followed by tarsal plate 202 (11.99%) and Iron 1,125 (66.80%) was the most
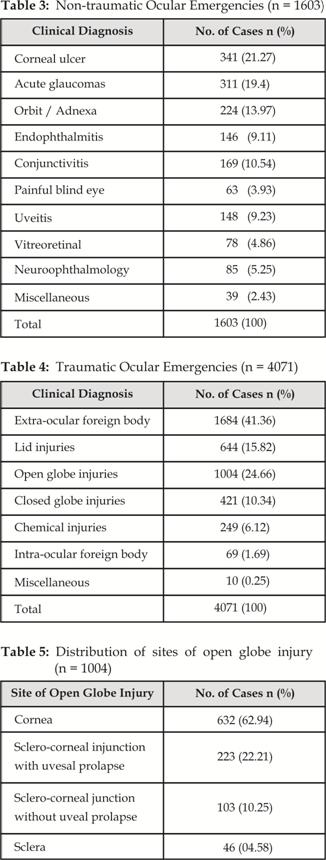
common foreign body followed by sand 286 (16.98). Among the open globe injury
825 (84.53%) episodes were due to accidents. Common source of accidental open
globe injury was due to stone 450 (54.55%) (Fig.2). Most common site of open
globe injury was cornea 632 (62.94%) followed by sclera-corneal junction with
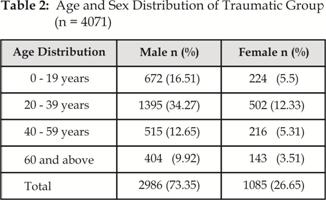
uveal prolapse 223 (22.21) (Table 5). Among closed globe injury cases 421 (10.34%)
hyphema 214 (50.83%) was the most common presentation (Table 6). Corneal ulcer
341 (21.27%) and acute glaucomas 311 (19.4%) were the leading causes of
non-traumatic group. Bacterial etiology 198 (58.06%) was the most common cause
followed by viral 94 (27.56%) (Fig. 1).
ETIOLOGY OF CORNEAL ULCER
Fig. 1: Showing etiology of Corneal ulcer among patients in Non-traumatic
group (n = 341)
Age and sex distribution of
non-traumatic and traumatic groups were shown in (Table 1, 2) respec-tively.
The frequencies of non-traumatic and traumatic ocular emergencies were shown in
(Table 3, 4) respectively.
DISCUSSION
An audit of surgical outcome can be seen as the final step in what
had been termed the “journey of care” for both the individual patient and for
the population as a whole6. Ocular emergency cases remain the
serious clinical problem and if not managed properly it could be sight threatening.
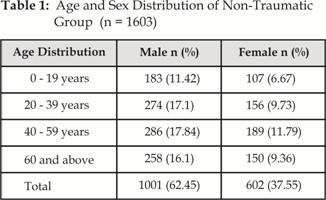
In our
study majority of the patients of non-traumatic ocular emergencies were middle
aged. This could be explained by the fact that certain diseases of older age
groups present as ocular emergency, such as lens induced glaucoma (LIG), and angle
closure glaucoma (ACG). Male Predominance was seen in both groups. In this
study we found that almost 1/3rd patient out of the total ocular emergency was
due to trauma. Trauma was a common ocular morbidity and damage may be
immediately apparent or may develop after the injury as a secondary
complication. However ocular trauma is mostly preventable by the use of
suitable eye protection7. Ocular trauma had greater potential to
cause permanent visual or cosmetic defect for rest of the life in the affected
individuals and was a major cause of monocular blindness and visual impairment
throughout the world, although little is known about its epidemiology or
associated visual outcome in developing countries8.
Khattak et al reported that
trauma as a common cause of unilateral blindness9. A national
population based survey of blindness in Nepal found a blindness prevalence rate
of 0.8% and trauma was responsible for 7.9% of monocular blindness10.
In our study majority of the patients belonged to 2nd-3rd decades, in which 2/3rd
of the total patients were males in the traumatic group. This finding
correlates with the finding of Al–Rajhi, et al, they reported that 77% of
ocular trauma occurred in males11.
Fig. 2: Showing sources of accidental Traumatic open globe injury (n = 825)
In the
present study commonest site of lodgment of extra-ocular foreign body was
cornea. Iron was the commonest foreign body followed by sand and agricultural
matter in order of decreasing incidence. In traumatic open globe injury cornea
was the most common affected part of eye followed by Sclera-corneal rupture
with uveal – prolapse. Asaminew T et al reported that cornea was the most
common affected part of the eye i.e. 63.2%, cornea – scleral injury 14.8%, and
uveal – prolapse or damage were 8.9%12. Accidental open globe
rupture being the most common which is similar to the findings with Vats S et
al, who reported that 87.1% episodes were due to accidents, 10.4% due to
alleged assault, and 2.5% were self-inflicted13. We also found that
hyphema was the most common presentation among the traumatic closed globe
injury. According to Fasih U et al 22.2% of the patients presented with hyphema
in their study14.
Chemical
injuries, though relatively less frequent are very devastating to the eye. In
our study it was not possible to classify the chemical induced injuries
according to the nature of the chemicals because no such documentation for such
cases was available. Ramakrishnan et al has shown that accidental chemical
injury at the work place is most common in the group of 19 – 30 years15.
Majority
of the extra ocular foreign bodies were removed. Closed globe and chemical
injuries were managed medically. In all cases of open globe injury, primary
repair was done. Valid estimation of the annual incidence of infective
ulceration was difficult to obtain in most countries8. In our study
we found that corneal ulcer was the most common non-traumatic ocular emergency.
Gonzales CA et al reported that annual incidence of corneal ulcer in Madurai
district, South India was 11.3 per 10,000 population16. Bacteria
were the most common etiologic agent followed by virus and fungus. Iqbal A et
al in their study reported that bacterial corneal ulcer were the most frequent
causes i.e. 63.4% followed by fungal 21.2% and viral ulcer were 12.1%9.
Bharathi MJ et al found that 32.77% were bacterial and 34.4% were fungal
corneal ulcer in their study17. These findings also support our
findings.
In all cases of non-traumatic
ocular emergencies, conservative medical management was given.
CONCLUSION
This study
indicates that ocular trauma is a significant cause of mono-ocular and
sometimes bi-nocular visual loss in all age groups. Many injuries and their
visual outcome may be prevented through education and prompt, appropriate
medical care. Health education and safety strategies can prevent most serious
ocular emergencies both at home and place of work. The incidence of
occupational ocular injuries can be reduced by mandatory use of protective goggles
and alcohol free environment at work place. Majority of the non-traumatic
ocular emergencies were corneal ulcers, mostly due to bacterial etiology. This
indicates that public health awareness about ocular hygiene and early
intervention of all cases of red eyes can considerably reduce the burden of
non-traumatic ocular emergencies. A 5 year retrospective clinical audit of
ocular emergencies in a rural hospital will definitely enable future health
managers and clinicians to formulate comprehensive strategies for prevention
and management of ocular emergencies both at the level of communities as well
as health care delivery units.
Author’s Affiliation
Dr. Subhasis Jana
MS (Final year) PGT
Department of Ophthalmology
Burdwan Amaedical College
Burdwan, West Bengal, India
P.O. Rajbati. PIN:
713104
Dr. Saumen kumar Chaudhuri
Assistant Professor
Department of Ophthalmology
Burdwan Amaedical College
Burdwan, West Bengal, India
P.O. Rajbati. PIN:
713104
Dr. Asim Kumar Dey
Associate professor
Department of Ophthalmology
Burdwan Amaedical College
Burdwan, West Bengal, India
P.O. Rajbati. PIN:
713104
Dr. Purban Ganguly
MS (First year) PGT
Department of Ophthalmology
Burdwan Amaedical College
Burdwan, West Bengal, India
P.O. Rajbati. PIN:
713104
Dr. Mousumi Bandyopadhyay
Professor and Head, Dept. of Ophthalmology
Burdwan Amaedical College
Burdwan, West Bengal, India
P.O. Rajbati. PIN:
713104
Dr. Subrata Dutta
Professor
Department of Ophthalmology
Calcutta National Medical
College
Kolkata, India
REFERENCES
1.
Alam SN,
Rehman S, Raza SM, Manzar S. Audit of a general surgical unit: Need for
self evaluation. Pak J of Surgery. 2007; 23: 141-4.
2.
Bilal A,
Salim M, Muslim M, Israr M. Two years audit of thoracic surgery
department at Peshwar. Pak J Med Sci. 2005; 21: 12-6.
3.
Karman
K, Antunica AG, Perk SR. Epidemiology of adult eye injuries in
Split-Dalmatian county. Croatian Medical journal 2004; 45: 304-9.
4.
Fea A,
Bosone A, Rolle T, Grignolo FM. Eye injuries in an Italian
urban population: report of 10, 620 cases admitted to an eye emergency
department in Torino. Graefes Arch Clin Exp Ophthalmol. 2008; 246: 175-9.
5.
Chaudhuri
SK, Jana S, Biswas J, Bandyopadhya. Modes and impacts of
agriculture related ocular injury. Int J Health Sci Res. 2014; 4: 108-11.
6.
Herbert
MA, Prina SL, William SJL. Are unaudited records forming an outcome
registry database accurate? Ann Thorac Surg. 2004; 77: 1960-4.
7.
Iqbal A,
Jan S, Khan MN, Khan S, Muhammad S. Admitted Ocular Emergencies: A
Four Year Review. Pak J Ophthalmol. 2007; 23: 58-64.
8.
Jackson
H. Bilateral blindness due to trauma in Combodia. Eye 1996; 10:
517-20.
9.
Khattak
MNK, Khan MD, Mohammad S, Mulk RA. Untreatable monocular
blindness in Pakistani eye patients. Pak J Ophthalmol. 1992; 8: 3-5.
10. Khatry SK, Lewis AE, Schein OD, et al. The
epidemiology of ocular trauma in rural Nepal. Br J Ophthalmol. 2004; 88:
456-60.
11. Al-Rajhi AA, Awad A, Badeeb O, Bwchari A. causes
of blindness in students attending schools for the blind in Saudi Arabia. Saudi
J Ophthalmol. 2003; 17: 276-80.
12. Asamanew T, Gelaw Y, Alemseged F. A
2-Year Review of ocular trauma in Jimma University Specialized Hospital. Ethiop
J Health Sci. 2009; 19: 67-74.
13. Vats S, Murthy GVS, Chandra M, Gupta SK,
Vashist P, Gogoi M. Epidemiological study of ocular trauma in an urban slum
population in Delhi, India. Indian J Ophthalmol. 2008; 56: 313-6.
14. Fasih U, Shaikh A, Fehmi MS.
Occupational ocular trauma (causes, management and prevention). Pak J Ophthalmol.
2004; 20: 65-73.
15. Ramakrishnan KM, Mathivanan T, Jayaraman V,
Babu M, Shankar J. Current scenario in chemical burns in a developing country:
Chennai, India. Ann Burns Fire Disasters. 2012; 25: 8-12.
16. Gonzales CA, Srinivasan M, Whitcher JP.
Incidence of corneal ulceration in Madurai District, South India. Ophthal
Epidemiol 1996; 3: 156-66.
17. Bharathi MJ, Ramakrishnan R, Vasu S,
Meenakshi R, Shivkumar C, Palaniappan R. Epidemiology of bacterial
keratitis in a referral centre in south India. Indian Journal of Medical
Microbiology. 2003; 21: 239-45.