Pterygium is one of the most common conjunctival
surface degenerative disorders seen in subtropical and tropical areas1-3.
Apart from causing cosmetics blemish, it alters the smoothness of the anterior
surface of the eye ball with disruption of the normal tear film. It can also
induce corneal astigmatism and if allowed to proceed over the pupillary area,
reduces the vision2. A number of different surgical approaches have
been proposed for the treatment of pterygium. The most common method has been
the bare scleral excision technique, first described by Ombrian4.
However, the major limitation to simple excision is the high rate of
postoperative recurrence5. Therefore a number of adjunct therapies
have been advocated along with excision to varying levels of success during the
last three decades. The use of topical Mitomycin C (MMC) as an adjunct therapy
to prevent pterygium recurrence has considerably increased since its first
introduction by Kunitomo and Mori of Japan6 and its subsequent usage
in US by Singh and associates7.
A
number of research studies have been carried out to document the appropriate
dosage and efficacy of MMC in treating pterygium and preventing its recurrence.
However relatively few studies have evaluated the role of other factors such as
age, gender, MMC exposure time, as well as the size and extent of pterygium
encroaching on the cornea8-10. Hence to prove the hypothesis that
the above mentioned factors also play an important role in pterygium
recurrence, we undertook this study to evaluate the role of these factors.
MATERIAL AND METHODS
This retrospective, case series study was carried at
Ophthalmology Department, Aga Khan University Hospital (AKUH), Karachi
Pakistan. The patients data files were analyzed starting from the period of
1999 till 2009. Only those patients fulfilling the following criteria were
enrolled in the study, informed consent from the patient, individuals of all
ages with established diagnosis of either unilateral or bilateral progressive
pterygia of different sizes, supervised surgical excision by bare scleral
technique and MMC administration, with minimum follow-up period of 12 months.
The patients lost to the follow up or having any suspicious growth other than
the pterygia and corneal scarring were excluded.
All patients had their detailed medical history
taken, with complete ocular examination including best corrected visual acuity
(BCVA), slit-lamp examination of anterior segment with Goldman applanation
tonometry and fundus examination with +90 DS lens. The pterygia were classified
either as primary or secondary on the basis of first time episode or recurrence
respectively.
The pterygium size was graded depending on the
extent of corneal involvement: Grade 1 pterygium encroaching over cornea for
2 mm. Grade 2 head of the pterygium covering cornea of more than 2 mm but
sparing the visual axis and Grade 3involving the visual axis.
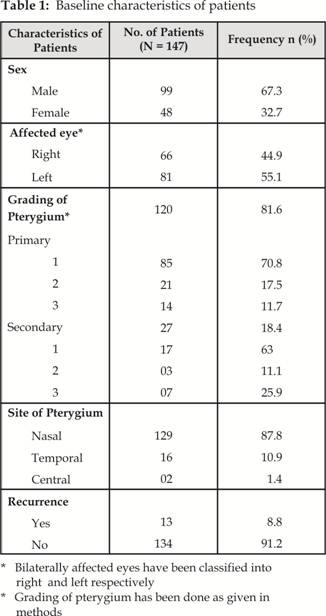
A total of 147 patients (147 eyes) based on our
inclusion criteria were incorporated in the study who had minimum follow up of
12 months, while 26 patients were lost to the follow-up, during the study
period were excluded from the study. Ninety-nine male and 48 female (Male to
Female ratio 2:1) aged between 16 and 60 years (mean age 46.4 years) were
included in the study. Primary pterygium was present in 120 patients while
secondary pterygium was diagnosed in 27 patients. One hundred two eyes (69.4%)
were affected by grade 1 pterygium, 24 eyes (16.3%) had grade 2 and 21 eyes
(14.3%) were having grade 3 pterygium. In 129 eyes (87.7%), pterygium was
located on the nasal side, with 16 eyes (10.9%) had it on the temporal side and
2 eyes (1.4%) were affected on the either side. Out of 147 eyes with pterygium,
66 belonged to the right eye and 81 to the left eye. The baseline
characteristics of patients are shown in (Table 1).
Pterygium excisions were performed on an outpatient
basis by the same surgeon using the same technique11. After excision
with bare scleral technique under topical anesthetic (Proparacaine Alcon
Belgium), a sterile sponge (5x5 mm) soaked in 8 10 drops of 0.2 mg/ml MMC
(0.02%) (Mitomycin C, Kyowa Japan) was applied over corneo-sclera and the
area from where pterygium was excised with variable duration of 1 5 minutes.
The sponge was removed and eye irrigated with 20 ml of Normal saline 0.9%. This
was followed by topical administration of Dexamethasone 0.1% + Tobramycin 0.3%
(Tobradex-Alcon, Belgium) and Hydroxypropyl Methylcellulose (Tear Naturale II
Alcon, Belgium) four times a day for 4 weeks. The dosage of MMC was calculated
in line with the international recommendations12-14. Patients were
regularly followed up at the interval of 3 months after the procedure. Any
Adverse effect or physical findings were noted on each visit for a minimum of
one year period. The recurrence of pterygium was defined as an encroachment of
fibrovascular connective tissue across the limbus and onto the cornea for any
distance in the position of the previous lesion.
The classification of subjects was done according to
the age, gender, MMC application time, type and grading of the pterygium.
Subjects were divided into two age groups (1) ≤ 50 years in age (2) > 50 years. The time duration of topical application
of MMC was divided into five groups, ranging from 1 to 5 minutes. The potential
factors were also classified accordingly (Table 2).
The study protocol was reviewed and approved by an
ethics committee at the study centre and the study was carried out in
accordance with the declaration of Helsinki of 1975 as revised in 1983. The
primary outcome measure was the comparison of pterygium affected eye for any
kind of recurrence after excision, along with the assessment of the potential
role of MMC and grading of the pterygium with other factors in pterygium
recurrence after a minimum of 12 months of follow up.
The
data was entered in Statistical Package for Social Sciences (SPSS) version 16 and
analyzed using frequencies, proportions, group means, standard deviation,
Pearson Chi square test and Fisher exact test. Alpha level of 0.05, confidence
interval of 95% and power of 0.8 were selected for the analysis.
RESULTS
Out of 147 eyes (147 patients), the recurrence of
pterygium was seen in 13 eyes (8.8%) of 13 patients with mean time of
recurrence of 6.77 months.
Out
of 13 recurrences, 12 patients were in the age group below 50 years (P = 0.04,
Pearson Chi Square test). Similarly there was a higher tendency of recurrence
in male (10.1%) as compared to female (6.2%) though this was not statistically
significant (P = 0.547). Most of the recurrence was seen on the nasal side
(9.3%) while 6.2% of pterygia recurred on either side (P = 1.00).
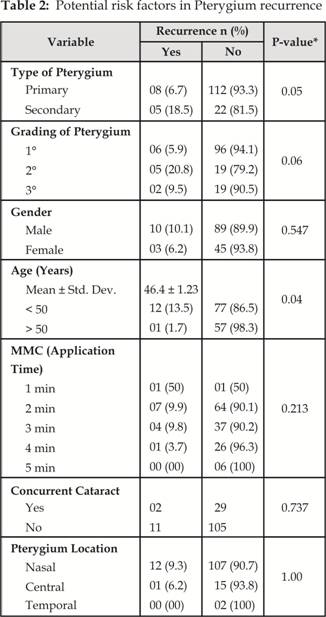
In the group with recurrent pterygia, the recurrence
rate was greater (18.5%) than in the group with primary pterygium (6.7%) (P = 0.05)
with mean (std.dev) time of 3.20 months as compared to 9.00 months. A definite
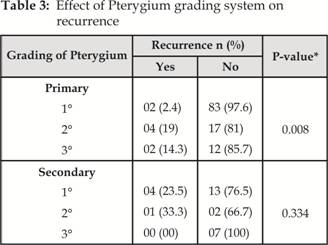
trend of recurrence was also noted on further stratification of the subjects on
the basis of the corneal involvement, with a higher rate of recurrence seen in
subjects with higher grades of corneal involvement (P = 0.06). Similarly, when
subjects with primary pterygia were graded according to the size, there was a
highly significant recurrence seen with higher grades of pterygium (P = 0.008).
However, the same was not seen in participants with secondary pterygia (P = 0.334).
The role of pterygium grading in recurrence of pterygiais shown in Table 3.
Mitomycin C application time was also noted for its relevance to the
recurrence and there was a decreased rate of recurrence from 50% in 1 minute
group to no recurrence seen in 5 minutes group (P = 0.213).
Corneal
nebular opacity was the frequent finding seen in most patients postoperatively
with one patient developing conjunctival cyst at the site of excision. No major
complication like scleral thinning, ulceration or necrosis was seen in our
patients.
DISCUSSION
The recurrence of the pterygium remains an important
health care issue in patients1 in Asian countries. The present study
was motivated by the invariably high recurrence of pterygium not only in
Pakistan but world over5, 15. The recurrence rate of pterygium in
the present study was 8.8%. In a recent clinical trial carried out in the
Pakistani population, Rahman et al16
estimated a recurrence of pterygia in 10% of the population. In another
prospective study, Cheng et al17
observed a recurrence of 7.9% in subjects with primary pterygia and a
recurrence of 19.2% in subjects with recurrent pterygia. However comparison
between our study and others is likely to be biased attributed to the different
study population, setting and criteria used for grading pterygium. The age was
significantly related to recurrence of pterygium in our study, with rising
cases of recurrence in younger age groups of < 50 years. Similar conclusions
have been drawn from various studies carried throughout the globe18-20.
The female gender was not related to recurrence in the target group, presumably
due to the fact that women in Pakistan are most of the time housewives whereas
men are commonly exposed to the occupational and environmental hazards, leading
to higher rate of recurrence.
The site of the pterygium was also investigated for
its role in recurrence, mainly because of the fact that in most of the cases,
pterygia is always present on the nasal side; however there was no significance
of site with recurrence.
The
secondary pterygium has been recognized as a risk factor for higher recurrence
in various studies17, 18, 19. Similarly, in the present study a
highly significant rate of recurrence of 18.5% was observed in the secondary
recurrent group as compared to 6.7% in the primary pterygium group. In a recent
prospective study carried out by Diaz et al21, no recurrence was
observed on follow-up in group of patient with previous recurrent pterygia
treated with intra-operative MMC. A lot of grading systems are currently being
used for grading pterygium but in our study we have used the grading system
based on the extent of corneal involvement by the fibrous pterygium. There was
a higher tendency of recurrence seen in participants with higher grades of
corneal involvement with rate of recurrence of 5.9% in 1° group as compared to
21% in 2° group. Similar results have been obtained in studies across Europe
where a high rate of recurrence has been associated with increased fleshiness
of the pterygia22, though the grading system used in these studies
is slightly different, with translucency and vascularity being used as a
criterion for grading. Nonetheless in both the studies, a higher grade is
increasingly being recognized as a risk factor for recurrence. In the secondary
pterygium group, the same results could not be achieved, though a definite
trend has been noted possibly due to the small sample size. The possible
difference in the effect on recurrence of pterygium by the application of
intra-operative topical MMC can be attributed to the difference in
concentration as well as its application time. In a dose response study related
to MMC, Robin et al23 have shown that duration of exposure appears
to be more important than the concentration of MMC. In the present study, there
was no recurrence seen in patients treated with topical MMC for 5 minutes,
however a high recurrence rate of 50% was seen in patients treated for 1
minute. Other groups had a recurrence rate in between these two extremities.
Similar results were also documented in a randomized trial carried out by Lam
et al15. In their work, at a mean follow-up time of 30 months, a
recurrence rate of 8.3% was seen in the patients applied 0.02% MMC for 5
minutes as compared to 42.9% seen in the group applied 0.02% MMC for 3 minutes.
Though there was no recurrence seen in the 5 minute MMC application group, most
cases of corneal nebular opacity were seen among these patients. The results of
our study hold important implications for further work on MMC, as probably,
duration of administration of MMC, holds the key in its effect on pterygium
recurrence.
CONCLUSION
Our
study found significant associations of recurrence with higher grade as well as
with secondary pterygia. There was a lesser recurrence with old age. The
results of this study, suggests using MMC application time of greater than 3
minute for high risk recurrent pterygia.
Authors Affiliation
Dr. P. S Mahar
Aga Khan University Hospital
Karachi
Dr. Nabeel Manzar
Aga Khan University Hospital
Karachi
REFERENCES
1.
Ang LP, Chua JL, Tan DT.
Current concepts and techniques in pterygium treatment. Curr Opin Ophthalmol. 2007; 18: 308-13.
2.
Gupta VP, Saxena T.
Comparison of single-drop mitomycin C regime with other mitomycin C regimes in
pterygium surgery. Indian J Ophthalmol. 2003; 51: 59-65.
3.
Mahar P S, Manzar N, Ahmad K.
The effect of intra-operative use of topical mitomycin c on intraocular
pressure in patients with pterygium excision. Asian J Ophthalmol. 2010; 12: 144-8.
4.
Ombrain A. The surgical treatment
of pterygium. Br J Ophthalmol. 1948; 32: 65-71.
5.
Hirst LW. The treatment of
pterygium. Surv Ophthalmol 2003; 48: 145-80.
6.
Kunitomo N, Mori S.
Studies on the pterygium. Part 4. A treatment of the pterygium by mitomycin C
instillation. Acta Soc Ophthalmol Jpn.
1963; 67: 601-7.
7.
Singh G, Wilson MR, Foster CS.
Mitomycin eye drops as treatment for pterygium. Ophthalmology. 1988; 95: 81321.
8.
Qing-feng L, Liang X, Xiu-ying J, Qi-sheng Y, Xiao-hui Y,
Tong-tong C. Epidemiology of pterygium in
aged rural population of Beijing, China. Chinese Medical Journal. 2010, 123:
1699-1701.
9.
Bradley JC, Yang W, Bradley RH, Reid TW, Schwab IR. The science of pterygia. Br J Ophthalmol. 2010; 94: 815-20.
10. Gazzard G, Saw SM,
Farook M, Koh D, Widjaja D, Chia SE et al. Pterygium
in Indonesia: prevalence, severity and risk factors. Br J Ophthalmol. 2002; 86:
1341-6.
11. Mahar PS, Nwokora GE. Role of mitomycin- C in pterygium surgery. Br J Ophthalmol. 1993;
77: 433-5.
12. Hayasaka S, Noda S,
Yamamoto Y, Setogawa T. Postoperative instillation of low dose mitomycin-c in the
treatment of primary pterygium. Am J Ophthalmol. 1988; 106: 7158.
13. Rachmiel R, Leibe H,
Levartovsky S. Results of treatment with
topical mitomycin C 0.02% following excision of primary pterygium. Br J
Ophthalmol. 1995; 79: 2339.
14. Panda A, Das G K, Tuli S
W, Kumar A. Randomized trial of
intra-operative mitomycin C in surgery for pterygium. Am J Ophthalmol. 1998; 125: 59-63.
15. Lam DS, Wong AK, Fan DS,
Chew S, Kwok PS, Tso MO. Intraoperative mitomycin
C to prevent recurrence of pterygium after excision: a 30-month follow-up
study. Ophthalmology. 1998; 105: 901-4.
16. Rahman A, Yahya K, Sharif
ul Hasan K. Recurrence rate of Pterygium
following surgical excision with intra operative versus postoperative
mitomycin-C. J Coll Physicians Surg Pak 2008; 18: 489-92.
17. Cheng HC, Tseng SH, Kao
PL, Chen FK. Low-dose intra operative
mitomycin C as chemo adjuvant for pterygium surgery. Cornea. 2001; 20: 24-9.
18. Chen PP, Ariyasu RG,
Kaza V, LaBree LD, McDonnell PJ. A randomized
trial comparing mitomycin C and conjunctival autograft after excision of
primary pterygium. Am J Ophthalmol. 1995; 120: 151-60.
19. Mastropasqua L,
Carpineto P, Ciancaglini M, Enrico Gallenga P. Long term results of intraoperative mitomycin C in the treatment
of recurrent pterygium. Br J Ophthalmol. 1996; 80: 288-91.
20. Mahar PS. Role of Mitomycin-C in Reducing the Recurrence of Pterygium after
Surgery. Pak J Ophthalmol. 1996; 12: 91-4.
21. Dνaz L, Villegas VM,
Emanuelli A, Izquierdo NJ. Efficacy and safety of
intra operative mitomycin C as adjunct therapy for pterygium surgery. Cornea.
2008; 27: 1119-21.
22. Tan DTH, Chee SP, Dear
KBG, Lim AS. Effect of pterygium morphology
on pterygium recurrence in a controlled trial comparing conjunctival autografting
with bare sclera excision. Arch Ophthalmol. 1997; 115:1235-40.
23. Robin A, Ramakrishnan R,
Krishnadas R, Smith SD,
Katz JD,
Selvaraj S,
Skuta GL,
Bhatnagar R.
A long-term dose-response study of
mitomycin in glaucoma filtration surgery. Arch Ophthalmol. 1997; 115: 969-74.