Retinal detachment is the separation of neurosensory retina
from the retinal pigment epithelium. Rhegmatogenous retinal detach-ment
involves a full thickness retinal break and accumulation of liquefied vitreous
under the neurosensory retina, separating it from the retinal pigment
epithelium1.
Various procedures are employed to treat rhegmatogenous
retinal detachment. All of them involve closing the break(s) by chorioretinal
adhesion, either by internal or external tamponade. The choice of procedure is
governed by many factors, primarily the location of the break, the amount of
proliferative vitreoretinopathy (PVR) and the availability of instrumentation
and expertise.
Eyes with minimal PVR and anteriorly located break(s) can be
successfully managed by pneumatic retinopexy, scleral buckle or vitrectomy
while eyes with posterior break(s) or significant PVR need vitrectomy along
with tamponading gas or oil2. The specific gravities of most of the
internal tamponading agents are less than balanced saline solution. That is why
oil or gas bubble floats at the top most position, pressing the retina and
providing a tamponade for superior retina. However, its effect on the inferior
retina is not enough to press the retina down to pigment epithelium layer and it
fails to provide a tamponade3. This poses a problem in managing
patients having high grade PVR and inferior breaks, since neither scleral
buckle nor vitrectomy alone can keep the retina attached.
Various
studies have been conducted on which procedure should be carried out for such
cases, with no general consensus. Some authors suggest carrying out vitrectomy
with internal tamponade alone4, followed by strict head posture,
while others have suggested scleral buckle and vitrectomy with internal
tamponade combined5. The protocol for such cases in our department
is to carry out scleral buckle plus vitrectomy combined with internal
tamponade, and we would like to share our experience of the results and
complications of this procedure.
MATERIAL AND METHODS
The
study was conducted in eye department of Lahore General Hospital, Lahore.
Patients were operated between January 2012 to June 2013, while post-operative
examination continued till December 2013. Thirty four patients having primary
rhegmatogenous retinal detachment, with inferior breaks between 4 o’clock to 8
o’clock positions were included in the study. All the patients were informed
about their inclusion in the study and a written consent was obtained. The
study was approved from the ethical committee of the hospital.
A
detailed pre-operative examination was carried out in all patients, with their
visual acuity, pupil reaction, intraocular pressure, slit lamp examination of
anterior segment, slit lamp and indirect ophthalmo-scopy of posterior segment,
status of the retina, grading of proliferative vitreoretinopathy (PVR), extent
of detachment and location of breaks noted.
The
exclusion criteria were: 1) patients with a past history of surgery for retinal
detachment. 2) Patients with detachment due to retinal dialysis. 3) Patients
with grade A PVR.
All
surgeries were performed by two experienced vitreo-retinal consultants. 360o
scleral encirclement was performed using a silicone band – 240, anchored at
12-14mm from the limbus. It was supplemented with an appropriate segmental
buckle (silicone tyre-277) to cover the retinal break(s). A 23-G, 3-port pars
plana vitrectomy was performed on each patient using Accurus vitrectomy system.
Silicone oil, 1000 centi-stokes (26 patients) or 5000 centistokes (8 patients),
was used for internal tamponading. Laser barrage around the break(s) was
applied in all patients. Post-operative examination was carried out on 1st
and 7th post operative days; and then after 1, 3 and 6 months and
status of retina noted on each visit.
Statistical analysis was done by using SPSS version
20. Descriptive statistics was used to analyse the data. A quantitative
variable like age was measured by mean and standard deviation. Frequency and
percentage was calculated for gender and surgical outcome in terms of retinal
attachment or non-attachment.
RESULTS
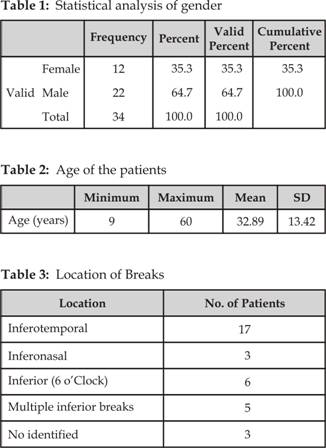
Thirty four patients fulfilling
the inclusion and exclusion criteria were identified from January 2012 to June
2013. 22 (64.7%) patients were male, while 12 (35.2%) were female (Fig. 1).The
statistical analysis of gender is shown in table 1. The mean age of the
patients was 32.88 with standard deviation of 13.42 (Table 2). In 17 patients,
the break was located inferotemporally, in 3 patients, it was located
inferomedially, in 6 patients, it was located inferiorly at 6 o’clock, while 5
patients had multiple breaks inferiorly. No definite break could be identified
in 3 patients due to poor peripheral visibility. However, their inferior retinas
showed diffuse degeneration and atrophic areas. The configuration of the
detached retina also corresponded to the presence of an inferior retinal
pathology (Lincoff rule), so they were supported with an inferior tyre and
included in the study (Table 3). Fourteen patients had grade B PVR, while
twenty patients had grade C PVR. Four patients had myopia of greater than -6
diopters while lattice degeneration was noted in 4 patients. 9 patients had
pseudophakia while 11 were aphakic and one patient presented with dropped IOL.
There was a history of trauma in 4 patients (Fig. 2).
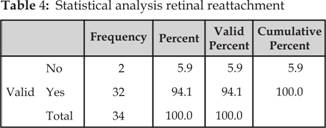
Successful attachment of the
retina was achieved in 32 (94.12%) patients, while 2 had persistent detachment
(Fig. 3). Out of the patients with grade B PVR (14), one developed grade C PVR
but his retina remained attached. The statistical representation of surgical
outcome in terms of retinal reattachment is shown in Table 4.
Gender
analysis (percentage)
Fig. 1: Gender analysis
Patients with Risk Factors
for RD
Fig. 2: Number of patients with
risk factors for Retinal Detachment
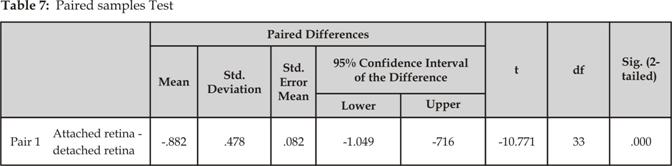
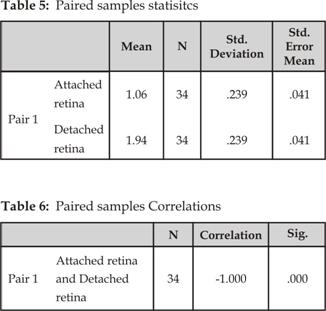
The findings were further analyzed by
the T-Test and the paired samples statistics, correlations and samples test are
shown in tables 5, 6 and 7 respectively.
Four patients (11.76%) had post-operative glaucoma while 3
patients (8.82%) complained of diplopia which resolved spontaneously. Three out
of the 13 phakic patients (23.08%) developed cataract within 6 months of the
surgery (Fig. 4).
Out of
the two patients with persistent retinal detachment following first surgery,
one patient had successful reattachment following a second surgery, while the
retina of one patient remained detached even after a second surgery.
DISCUSSION
Current
surgical techniques can obtain high rates of anatomical and visual success in
patients with retinal detachment6. However, the management of
retinal detachment with inferior break(s) has been the focus of debate
recently. The nature of the internal tamponading agents, due to low specific
gravity than normal saline, does not serve to tamponade the inferior retina
against the choroid. Some authorities advocate pars plana vitrectomy with
internal tamponade alone, along with strict post operative posturing in cases
of inferior retinal breaks in which buckling alone is not sufficient (e.g. high
grade PVR). They argue that combining scleral buckling does not add any
additional advantage over vitrectomy alone and poses the patient to additional
risks of scleral buckling like diplopia7, explant extrusion,
infection8 and choroidal haemorrhage. One such argument has been
given by Wickham and associates4.