Glaucoma is the major cause of irrevocable blindness1,7.
The incidence rate and preva-lence of glaucoma in Pakistan is similar to that
of other dark colored population of the developing countries, but tangible
statistical data is lacking. According to a study carried out in Lahore, 23% of
the blindness is found to be due to glaucoma6.
Long term medical treatment is improbable, however,
because of the long distances patients must travel for treatment, the high cost
and low accessibility to medications. Glaucoma is often taken to be a surgical
problem. Trabeculectomy with anti metabolites is an effective treatment for
POAG1,7. Primary trabeculectomy is still a procedure of choice all
over for cases in which a great lowering in IOP is the intent of the treatment,
especially when high IOP persists despite of giving maximum tolerable anti
glaucoma medication (which varies from patient to patient)2,8.
Diode Laser Trans-scleral Cycloablation (DLCA) has been
used effectively for the cure of refractory glaucoma, as well as those eyes in
which other surgical treatments have failed1,7. Diode laser is
widely established as the remedy of choice in severe glaucoma cases and is
appropriate as a primary surgical procedure4,5.
In
developing countries, there is a scarcity of both ophthalmologists and
resources for eye care. Regrettably, medical and surgical treatment cannot be
accessible to every glaucoma patient. Therefore, DLCA is an easy, swift and low
cost surgical procedure for patients with POAG after maximum endured medical
treatment. Diode laser is a harmless, efficient method to reduce the IOP in the
treatment of different glaucomas with few severe complications.
MATERIAL AND
METHODS
Sixty
patients satisfying the inclusion criteria were chosen from the Glaucoma Unit
of Layton Rahmatullah Benevolet Trust (LRBT) Hospital to be included in this
study. The duration of study was one year which included six months of
recruitment and six months of follow-up. After taking well versed permission,
socio-demographic data (name, age, sex, occupation) was recorded. A complete
ophthalmological history was taken. Preoperative and postoperative evaluation
was done by including visual acuity with Snellen Chart, IOP with Goldmann
applanation tonometer and Topcon air puff. Slit lamp examination with Haag
streit BQ-900 was done for anterior segment examination. Super field 90 D lens
was used for fundus evaluation including cup-disc ratio. Gonioscopic evaluation
of anterior chamber angle with Goldmann triple mirror and perimetry with
Humphry Visual Field Analyser was also done.
Inclusion Criteria were Primary Open Angle Glaucoma and
Maximum tolerated oral / topical medication while Exclusion criteria were
Uveitis, Cataract, Diabetes Mellitus, Hyper tension.
Treatment course of action included preoperative
administration of peribulbar or subtenon anesthesia. Transscleral Diode Laser
Cyclophotocoagulation (cyclodiode) was performed using the Iridis Quantal.
Laser was applied for 1.5 seconds with power between 1500 to 2000 mw. The power
was adjusted until a popping sound was heard and then reduced to just below
that level. Approximately 30 burns were placed 1.5 mm posteriorly to the limbus
over 270 degrees. Oral NSAIDS, topical dexamethasone 0.1% eye drops along with
anti glaucoma medication were continued for the 1st week. Miotics
were discontinued for the 1st week. Anti glaucoma medication was
tapered according to the drop in IOP. At 1 week post laser treatment oral acetazolamide
was discontinued if the lOP was < 21 mm Hg. Oral acetazolamide was given to
eighteen patients and was continued for up to one week. Topical steroids,
usually dexamethasone 0.1% eye drops, were given four times a day for 2 4
weeks after treatment. Follow up was noted on 1st day, 1st
week, 1st month, 6th month and 1 year.
Pre-op gonioscopic examination revealed POAG Grade III in
all the patients. Visual acuity and Visual Field remained unchanged in all the
patients.
Any
complications occurring in patients like anterior segment inflammation,
cataract, hyphema and hypotony were also taken into account.
RESULTS
Sixty patients were included in the study. Their ages
ranged between 45 to 60 years and the mean age of patients was about 52.73 ±
7.40 years. 60% of the patients were male and 40% were female. 52% operated
eyes were right and 48% were left eyes. Most of the patients were using three
or more anti-glaucoma drugs pre-op (Figure 1).
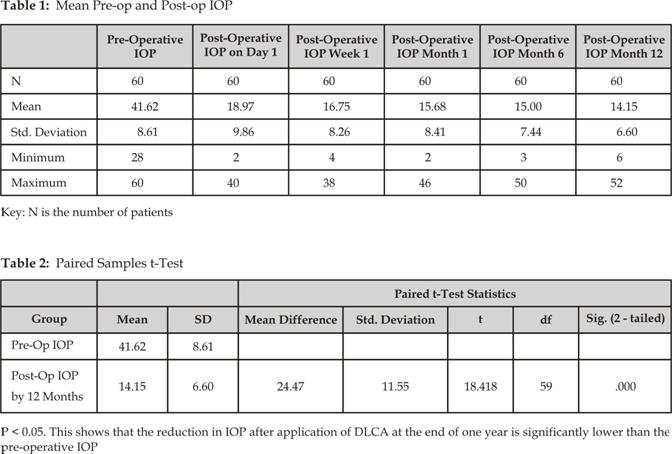
The mean pre-operative IOP was ± 41.62 mm Hg (The
pre-operative IOP ranged from 28 mm Hg to 60 mm Hg). The mean post-operative
IOP was 18.97 mm Hg on day one, 16.75 mm Hg at 1 week, 15.68 mm Hg at 1 month,
15.00 mm Hg at 6 months and by the end of a year it was about 14.15 mm Hg (The
post-operative IOP ranged from 6 mm Hg to 52 mm Hg). Mean post-operative IOP
lessened by more than 50% as compared to mean pre-operative IOP (Figure 2).
(The post-operative IOP ranged from 6 mm Hg to 52 mm Hg) (Table 1).
The mean post-operative IOP continued to decrease by the
end of one year. Anterior segment inflammation was seen in only eight eyes
(13.3%) out of 60 eyes. Similarly cataract as a complication occurred in 8 eyes
(13.3%), hyphema in 5 eyes (8.3%) while 6 eyes (10%) developed hypotony. We had
a maximum of 3 sessions in our series. Retreatment was done in 44% of which
only 6% received 3 treatment sessions.
Preoperative
and postoperative mean intra ocular pressure was assessed using paired t test
and final P values were 0.00 which is less than 0.05, and this shows that the
test is highly significant (Table 2).
Number of Anti Glaucoma Medications
being used prior to DLCA
Fig.
1: Most of the patients were using three
or more anti-glaucoma drugs pre-operatively.
![]()
Fig. 2: Drop of mean IOP following DLCA
This
proves that IOP decrease after DLCA by the end of one year is notably lower
than the pre-operative IOP. The complications with DLCA were evaluated using
chi square test, that included anterior segment inflammation, cataract, hyphema
and hypotony, and it showed that the minimum expected frequency is 30.0, and P
value for each complication is 0.00 which is less than 0.05, showing that the
complication rate is not significant.
DISCUSSION
In this study of DLCA as primary treatment for POAG, the
treatment was rapid and straight forward. Patient reception of treatment was
exceptional and patient. DLCA is relatively safe as no major complications came
into account.
DLCA has established itself a satisfactory track record
for the treatment of refractory glaucoma9-12. It has also been tried
as a primary surgical treatment in different types of glaucoma13-15.
The complications are tolerable. Inconsequential and transitory complica-tions
like pain and inflammation were noted by most authors16-18. Some
surgeons are trying it as an alternative to drainage implant surgery in complex
glaucoma19.
A constraint of the study may be that the group had a
small number of 60 patients. However, adequate follow-up information from all
patients was acquired and the cases were included on consecutive basis.
No standard protocol has yet been agreed upon for the
energy settings. Different settings have been used ranging from 1.5 Watts to
2.5 Watts for 1 2 seconds20-22. We used a power of 1500-2000 mw
titrating with the pop sounds. Spencer and Vernon used a fixed setting and did
not alter it to hear the pop sound3.
3 and 9 o clock positions should be avoided to save
ciliary nerves and in phakic eyes the probe must be 1.5 mm posterior to the
limbus to avoid lens damage.
Structural changes occurring with diode laser
trans-scleral photocoaggulation are thermal coagulative necrosis of ciliary
epithelia and stroma followed by atrophy, fibrosis and fusion of ciliary processes.
Oral NSAIDS, topical dexamethasone 0.1% eye drops along with anti glaucoma
medication except miotics were continued for the 1st week. Anti
glaucoma medication was tapered in accordance with the drop in intraocular
pressure. At 1 week post laser treatment oral acetazolamide was discontinued if
the lOP was < 21 mm Hg. Topical steroids, usually dexamethasone 0.1 %
eye drops, were prescribed four times a day for 2 4 weeks after treatment.
We had a mean drop of 50.08% in IOP. This is comparable to
other studies mentioned above where a decrease of 20 65% in mean IOP has been
reported.
There
is no agreement on how many times the procedure should be repeated. Spencer and
Vernon repeated the procedure up to five times22. We had a maximum
of 3 sessions in our series.