Intraocular
foreign bodies (IOFBs) represent a subset of ocular injuries that present
complex surgical challenges for successful removal while preserving the vision,
restoring ocular architecture and preventing complications.
Studies have reported that an IOFB may be
present in 14% to 45% of cases of penetrating injuries of the globe1, 2.
Removal of posterior segment IOFBs by vitrectomy is advocated because it
provides direct viewing and also precise removal of the IOFB2. Vitrectomy,
by removal of blood in the vitreous, prevents inflammatory and fibrous
responses that may lead to tractional sequelae in the posterior segment3,4.
The hammer-chisel injury is the most common cause of IOFB in adults5.
The IOFB most commonly causes damage to the eye by mechanical ways,
introduction of infection and specific chemical reaction in the intraocular
tissues6, 7.
In this particular study we
present our experience with posterior segment IOFB removal with endomagnet plus
intraocular forceps vs intraocular forceps alone. Thus ocular trauma with an
IOFB is an important cause of ocular morbidity and blindness and is often under
reported
MATERIAL AND METHODS
This
was a comparative case-series conducted at Mayo Hospital, Lahore. The study was
carried out over a period of six months from March to August 2013. Fifty eyes
of fifty patients with ocular trauma and concurrent metallic posterior segment
intraocular foreign body underwent pars plana vitrectomy and we studied the
ease of removal of posterior segment IOFB with intraocular forceps or
endomagnet plus forceps. The ease of removal was judged by the various
per-operative difficulties / complications encountered during the
removal of the IOFB. The patients randomly were assigned into two groups: Endomagnet
plus forceps (EF) and Forceps alone (F). We used a 20 G crocodile forceps and a
permanent retractable endomagnet.
An
IOFB was suspected in all cases of open globe injuries. The preoperative workup
included a dedicated history to determine the time lapsed and modality of
injury along with detailed data about the composition of the object. A careful
ocular examination with minimal manipulation of the globe to avoid further
expulsion of its contents was done. If view to the posterior pole was limited,
gentle B-scan ultrasound by an experienced ultrasonographer was arranged
ensuring that no pressure was applied to the globe. CT scan was done in
selected cases to further aid in identifying the objects and evaluating the
globe, orbital bones and retrobulbar space.
The surgical technique
employed was a standard three port pars plana vitrectomy with simultaneous pars
plana lensectomy or phacoemulsification if and when considered necessary. After
identification of IOFB, core vitrectomy and induction of PVD was performed. The
IOFB was then removed by forceps alone or elevated from the retinal surface by
an endomagnet and then grasped with forceps as the magnet is not able to hold
the IOFB during its passage through the sclerotomy. For the changeover from
magnet to forceps, the endomagnet tip was brought just behind the lens, kept in
view with the help of microscope light. An intraocular foreign body forceps was
then inserted through the other sclerotomy. In cases where there was inadequate
view through the pupil, we used a self-retaining 25G Awh chandelier
(synergetics, inc) for illumination. This was inserted through a separately
created 4th port with a 25G MVR. We used perfluorocarbon intra operatively
to protect the macula and silicone oil as postoperative intraocular tamponade,
if required. Endolaser photocoagulation of the breaks and 360 degree
photocoagulation of the retinal periphery were performed. Before securing the
IOFB, the route of removal was planned so that either the sclerotomy was
enlarged or a keratome incision created to remove the IOFB through the limbus
in aphakic patients.
RESULTS
Fifty
eyes of fifty patients (all male with a mean age of 38; age range 22 to 50
years) were treated during this study period.
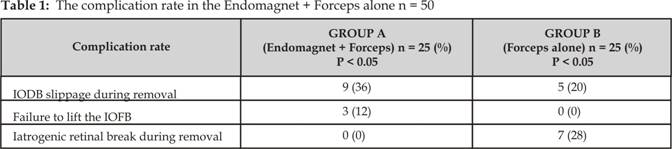
In our
study we assessed the ease of removal of IOFB by comparing the complication
rates of the two methods under discussion.
The
IOFB slipped during removal in 9 (36%) of the 25 patients in Group A while
slippage occurred in only 5 (20%) of the patients in Group B. In 3(12%) cases
in Group A there was failure to lift the IOFB during removal with the
endomagnet predominantly due to the large size of the IOFB; however such a
complication was not encountered with the group B. One of the drawbacks of
using forceps is iatrogenic retinal break due to the sharp edges of the various
foreign body forceps coming in contact with the retinal surface. This
complication was encountered in 7 (28%) of the 25 cases in Group B; in
contrast, none of the patients in group B encountered this complication (Table 1).
DISCUSSION
PPV for removal of IOFB often presents a formidable surgical
task. However, the final results can be favorable, despite the serious nature
of the initial injury8-10. The most common location for a retained
intraocular foreign body is within the vitreous cavity11.
Like other traumatic injuries to the eye, occurrence of
IOFBs is effectively prevented by strict adherence to the recommended safety
measures because most of them are occupational 12, 13. Some of the
activities like hammering metal on metal and chiseling related activities have
a relatively high probability of producing high velocity projectiles that can
enter and damage the globe14. War injuries also have a high
probability of IOFBs15.
Although occasionally other tools may
also be utilized e.g., paper clips, catheter, snare16, 17 there are
three basic types of instruments for IOFB removal: External Electro Magnets
(EEMs), Intraocular forceps and Intraocular Magnets (IOMs)18. EEMs
may be equipped with intraocular attachments but they are bulkier and less
convenient to use than IOMs19.
The inherent problem of the EEM is that
the surgeon has to view the removal process from an angle, making it difficult
to align the following:
·
External magnetic pole.
·
Surgical incision / instrument tip.
·
IOFB.
The potential for complications is
significant. The EEM also has a tendency to overheat, reducing efficiency and
possibly burning the patients skin. The weight (up to 1 ton) can cause
logistical difficulties.
Intraocular Forceps allow controlled
maneuvers but may require considerable dexterity to grasp the IOFB (e.g.,
lifting up sharp objects from the retinal surface) or to adjust its position
(e.g., aligning the IOFBs longest axis with that of the instrument) 20.
Use of additional tools such as heavy liquids provides limited help.
The Intraocular Magnets are permanent magnets that allow
controlled IOFB removal with no need for special dexterity. Free-flying of the
IOFB, inherently considerable with EEMs is ≤ 2 mm. However, most IOMs
gradually lose power with time and have a limited pull force, commonly
requiring concurrent forceps use19.
The aim
in managing an IOFB is to achieve the best visual outcome possible by
identifying and closing the entry and exit sites, reconstructing the eye and
removing the object.
CONCLUSION
The primary goal in managing IOFB is to preserve vision. The
best instrument to use for removal depends on the size, shape and magnetic
properties of the IOFB as well as its location within the eye.
Authors Affiliation
Dr. Tehmina Jahangir
Vitreo-retinal fellow
Eye Department
KEMU / Mayo Hospital, Lahore
Dr. Bilal Zaheer Qureshi
Vitreo-retinal fellow
Eye Department
KEMU / Mayo Hospital, Lahore
Dr. Qasim Lateef Chaudhry
Assistant Professor
Eye Department
KEMU / Mayo Hospital, Lahore
Prof. Dr. Asad Aslam Khan
Professor of Ophthalmology
Eye Department
KEMU / Mayo Hospital, Lahore
REFERENCES
1.
Ehlers JP, Kunimoto DY, Ittoop S, Maguire JI, Allen C, Regillo CD.
Metallic Intraocular Foreign Bodies: Characteristics, Interventions and
Prognostic Factors for Visual Outcome and Globe Survival. Am J Ophthalmol.
2008; 146: 427-33.
2.
Yeha S,
Colyerb MH, Weichel ED. Current trends in the management of
intraocular foreign bodies. Curr Opin Ophthalmol. 2008; 19: 225-33.
3.
Katz G,
Moisseiev J. Posterior-segment intraocular foreign bodies: An update on
management. Retinal Physician. April 2009: 1-9.
4.
Demircan
N, Soylu M, Yagmur M, Akkaya H, Ozcan AA, Varinli I. Pars
plana vitrectomy in ocular injury with intraocular foreign body. J Trauma.
2005; 59: 1216-8.
5.
Falavarjani
KG, Hashemi M, Modarres M, Parvaresh MM, Naseripour M, Nazari H, et al.
Vitrectomy for Posterior Segment Intraocular Foreign Bodies, Visual and
Anatomical Outcomes. Middle East Afr J Ophthalmol. 2013; 20: 244-7.
6.
Kuhn,
Ferenec (Editor). Ocular Trauma: Principles and Practice. New York, NY, USA:
Thieme Medical Publishers, Incorporated, 2002: 235-63.
7.
Wani VB, Al-ajmi M, Thalib L.
Vitrectomy for posterior segment intraocular foreign bodies, visual results and
prognostic factors. Retina. 2003; 23: 654-60.
8.
Greven
CM, Engelbrecht NE, Slusher M, Nagy SS. Ocular foreign bodies:
management, prognostic factors and visual outcomes. Ophthalmology 2000; 107: 608-12.
9.
Zafar S,
Kamil Z, Shakir M, Bokhari SA, Rizvi SF. Management of Intraocular
Foreign Body in Tertiary Care Hospital. Pak J Ophthalmol. 2012; 28: 118-21.
10.
Woodcock
MG, Scott RA, Huntbach J. Mass and shape as factors in intraocular
foreign body injuries. Ophthalmology 2006; 113: 2262-9.
11.
Chow DR,
Garretson BR, Kuczynski B. External versus internal approach to the
removal of metallic intraocular foreign bodies. Retina 2000; 20: 364-9.
12.
Iqbal M.
Consensus Report. Retained Intraocular Foreign Body. Pak J Ophthalmol. 2010; 26:
158-61.
13.
Memon
AA, Iqbal MS, Cheema A, Niazi JH. Visual outcome and
complications after removal of posterior segment intraocular foreign bodies
through pars plana approach. JCPSP. 2009; 19: 436-9.
14.
Sriprakash
KS, Sujatha BL, Kesarwani S. Surgical intervention in retained
intra-ocular foreign body: Our experience. Retina/Vitreous Session 2. AIOC 2006
Proceedings; 493-5.
15.
Thach AB, Ward TP, Dick II JS, Bauman WC,
Madigan Jr WP, Goff MJ, Thordsen JE. Intraocular foreign body injuries during Operation Iraqi
Freedom. Ophthalmology. 2005; 112: 1829-33.
16.
Yao Y,
Wang ZJ, Yan S, Huang YF. An alternative method of extraction: use
of a catheter to remove intraocular foreign bodies during vitrectomy. Retina
2009; 29: 552-5.
17.
Erakgun
T, Akkin C, Mentes J. Management of the posterior segment foreign bodies with a simple
snare. Retina 2003; 23: 858-60.
18.
Pieramici
DJ. Open globe injuries are rarely hopeless. Managing the open globe
calls for creativity and flexibility of surgical approach tailored to the
specific case. Review of Ophthalmology. 2005; 12: 6.
19.
Erakgun
T, Egrilmez S. Prognostic factors in vitrectomy for posterior segment
intraocular foreign bodies. J Trauma. 2008; 64: 1034-7.
20.
Szijarto
Z, Gaal V, Kovacs B, Kuhn F.
Prognosis of penetrating eye injuries with posterior segment intraocular
foreign body. Graefes Arch Clin Exp Ophthalmol. 2008; 246: 161-5.