Orbital masses can be inflammatory, infectious and
neoplastic in origin. In orbital space, they present with overlapping clinical
manifestations. The slow growth of a solitary, discrete mass is usually
suggestive of tumor. Fungal infections of the orbit are usually seen in immune
compromised state1. But here, we report a case of orbital fungal
granuloma in a young female who was immune-competent and managed
satisfactorily.
CASE
REPORT
A 20 years old unmarried female,
presented to our tertiary care hospital with painless progressive non-axial proptosis of the left eye for the last 1 year. She had
outward deviation of the left eye with no double vision. She had no visual
complaints, no complaints of redness, discharge and photophobia. There was no
history of trauma, surgery, systemic illness, lymphadenopathy and nose or
throat infection. She had no fever and reported no change in appetite or
weight. Past medical and surgical history was unremarkable. She reported no
evidence of a disease causing immune suppression. Family history was
unremarkable.
On examination, visual acuity was 6/6 unaided in both eyes.
There was non-axial proptosis of 23 mm of the left
eye on Hertels exophthalmometer,
which increased slightly on Valsalva maneuver. She had an exotropia
of 45 degrees on cover test. The dystopia was measured to be 5 mm outwards and
5 mm upwards in the left eye (Fig 1). There was no complaint of diplopia. Bruit
and pulsation were absent. Anterior segment
examination was normal.

Fig. 1: proptosis and exotropia
of left eye on initial presentation.


Fig. 2: CT scan coronal and axial view showing mass involving
medial rectus.
Laboratory
findings revealed normal blood count, blood glucose level, PT and APTT.
Ultrasound abdomen and x-ray chest were of no significance. Computed tomography
of orbits and PNS revealed, diffuse thickening of medial rectus (Fig. 2). Rest
of the left eye appeared normal. Right eye, nasal cavity and sinuses were
within normal limits.
MRI orbit
showed thickening of medial rectus muscle and involvement of retrobulbar fat with proptosis of
left eye and compression of optic nerve Fig. (3). Brain appeared normal.
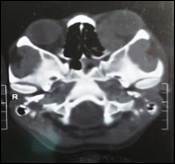
Fig. 3: MRI axial view showing the mass invading the medial rectus.
These findings gave the impression of a mass involving the
medial rectus. Surgical excision was performed under general anesthesia. Lynch Howarth approach was used. The excised mass which was
yellowish in colour unlike the medial rectus on naked
eye examination was excised and wound closed with 6/0 vicryl
(Fig 4). But the medial rectus tendon was forming the anterior end of the mass
which suggested that the muscle had lost its characteristic appearance due to
pathological changes. The tendon was identified and separated from the sclera
with a muscle hook before excision. Biopsy specimen was sent for histopathology
(Fig. 5).

Fig. 4: The tumour being removed.

Fig. 5: Biopsy specimen.
On a follow up
examination, 2 weeks after surgery, proptosis was
decreased to 20 mm. Optic disc, anterior and posterior
segments were within normal limits. Intraocular pressure was 16 mm Hg. Inward
eye movements were restricted (grade -4), but normal on superior, inferior and
lateral gaze (Fig. 6). There was no diplopia.

Fig. 6: Left exotropia with absent
abduction at 2 weeks Post op.
Histopathology report showed fibro-connective
tissue with granulomatous inflammation. Granulomas were composed of aggregates
of epitheloid cells, surrounded by collar of
lymphocytes and histiocytes with multiple
multinucleated giant cells within the granuloma. Scattered eosinophills
were also identified. Few granulomas showed septate
hyphae. Histochemical stains were positive for fungal
organisms.

Fig. 7: Post op CT showing residual fungal granuloma.
The proptosis
decreased after 2 weeks, but there was no movement of left eye on medial gaze,
due to absent medial rectus muscle and exotropia of
45 degrees was seen. Post op CT and MRI scans were carried out. They showed
residual fungal granuloma (Fig. 7). Patient was prescribed tablet Itraconazole(
sporonox) 100 mg twice a day for 3 months. After 3
months, CT and MRI were again carried out, which showed no recurrence of fungal
granuloma.
Cosmetic squint correction was done for the large angle exotropia by performing Hummulsheim
procedure. In this procedure, there was full tendon transfer of superior and
inferior recti to the medial rectus. A Jenson procedure involving split tendon
transfer could be done but we opted for full tendon transfer due to the very
large angle exotropia. Lateral rectus recession was
not feasible due to the absence of medial rectus which would pull it medially
after surgery. Post-op examination after 4 weeks showed improvement of exotropia on primary position to 30 degrees (Fig. 8).

Fig. 8: Residual small angle exotropia of
left eye at 4 weeks post op.
DISCUSSION
In adults, primary orbital tumors are
lymphoid tumors, cavernous hemangioma, meningioma, neurofibroma and schwannoma. Most
common presentations are proptosis and exophthalmos.
Infectious and inflammatory process has acute onset as compared to tumors,
which has slow onset. In the presented case fungal granuloma developed in an
immune competent patient over a period of 1 year with no acute symptoms except proptosis.
Orbital infections occur due to spread
of infections from paranasal sinuses or direct from
trauma and surgery. Most common organisms are bacteria, while viral and fungal
infections are rare. Organisms causing fungal infections include aspergillus. Mucormycosis and Cryptococcus species2. Aspergillus
granuloma is the most commonly reported intracranial granuloma among fungal
granulomas3. It is the common causative fungal organism of
intracranial fungal mass lesion accounting for approximately 56% to 69%3.The
estimated annual incidences of systemic invasive fungal infections caused by Aspergillus species are 12-34%4. The estimated
incidence of fungal infection is 4-6% of CNS involvement5.
Fungal infections commonly occur in immune compromised state like diabetes
mellitus (37%)6, AIDS or excessive steroid
use. The common sites of involvement are nasal cavity (10%), brain with sinonasal (36.6%) and nose and orbital cavity (53.3%)7. Some of the reports shows
that the fungal infections can present as optic neuritis8. It can present
in the form of sub periosteal abscess9. Optic
neuropathy8, orbital apex syndrome10 and orbital
tuberculosis with coexisting fungal granulomas11.
To assess the orbital disease, MRI
imaging is preferable because it gives full detail of the soft tissue
structures. The MRI findings are characteristics in fungal granuloma. These
include a mass lesion producing hypo-intense or iso-intense
lesion on T1 weighted and hypo intense lesion on T2
weighted images12.
In our case, MRI findings of fungal
granuloma on T1 weighted images were iso-intense
while they were hypointense on T2 weighted
images, which in literature are characteristic of aspergillus
fungal granuloma. Its non-tender and non-inflammatory nature caused it to be misdiagnosed
as tumor. So, fungal infections should always be kept in differentials of such
solitary orbital masses.
Surgery is important both for initial diagnosis and for
excision of granuloma, allowing for a better treatment efficacy of systemic
antifungal agents like Amphotericin B and Itraconazole
100-400 mg twice a day for 3 months.
CONCLUSION
Orbital fungal granuloma may affect immune competent healthy
patients as well as immune compromised patients. Main stays of treatment are
surgical debridement and systemic antifungal therapy. Early diagnosis can
prevent the extensive surgical intervention.
Authors Affiliation
Dr. Saher Khalid
PGR Eye
Unit 2
lahore General Hospital
Lahore
Dr.
Mohammad Moin
Professor
Ophthalmology
Eye
Unit 2
Lahore
General Hospital
Lahore
REFERENCES
1.
Zafar MA, Waheed
SS, Enam SA. Orbital aspergillus infection
mimicking a tumor: a case report. Cases journal. 2009; 2: 7860.
2.
Hershay BL, Roth TC. Orbital infections. Semin ultrasound CT
MR 1997; 18: 448-59.
3.
Sundram C, Umabala P. Pathology of fungal infections of
central nervous system: 17 years experience from Southern India. Histopathology.
2006; 49: 396-405.
4.
Pfaller MA. Pappas PG. invasive fungal pathogens, current epidemiological
trends. Clinical infectious disease. 2006; 43: 3-14.
5.
Kethireddy S, Andes D. CNS pharmacokinetics of antifungal agents. Expert Opinion on Drug
Metabolism and Toxicology. 2007; 3: 573-81.
6.
Finn DG. Mucormycosis
of paranasel sinuses. Ear Nose Throat J. 1998; 67:
813-16.
7.
Javadi M. Fungal infection of the sinus and anterior skull base. Med J
Islam Repub Iran. 2008; 22: 137-40.
8.
Mafee MF, Goodim J. optic nerve sheath meningiomas.
RadiolClin North Am. 1999; 37: 37-58.
9.
Spoor TC, Hartel
WC. Aspergillosis presenting as a corticosteroid responsive
optic neuropathy. J Clin Neuroophthalmol.
1982; 2: 103-7.
10.
Matsou T, Notohara K. aspergillosis causing bilateral optic neuritis and
later orbital apex syndrome. Jpn J Ophthalmol. 2005; 49: 430-1.
11.
Reddy SS, Penmmaiah
DC.
Orbital tuberculosis with coexisting fungal infection. Surg
NeurolInt. 2014; 5: 32.
12.
Siddiqui AA, Bashir SH. Diagnostic MR imaging features of craniocerebralaspergillosis of sino
nasal origin in immune competent patients. Acta Neurochir. 2006; 148: 155-66.