Primary Congenital Glaucoma is a worldwide diagnostic and
therapeutic challenge. It is responsible for 0.01 – 0.04% of total blindness
and 5% of childhood blindness.ą It is an unusual, inherited anomaly of
trabecular meshwork and anterior chamber angle which leads to obstruction of aquous outflow, increased IOP, and optic nerve damage.˛
Incidence varies worldwide, as low as 1:20000-30000 live births in western
countries, as high as 1:1250 live births in Roman Slovakian.3 It is
typically bilateral (70 - 80%) with male (60%) preponderance. The high
incidence is related to parental consanguity.4 Pathogenesis
is still disputed; most observers have not been able to document
ultra-structurally a continuous endothelial membrane, as initially advanced by
Barkan.5 It is an isolated trabeculodysgenesis.
It is know thought to be due to thick, compacted trabecular sheets.6
It is typically autosomal recessive7. Medical therapy is
accorded a supportive role, definitive treatment is surgical. Both goniotomy and trabeculectomy give similar good results. Goniotomy clinically introduced by Barkan
in 1940s was undoubtedly a great step forward in the surgical management of
congenital glaucoma. However, good visibility of chamber angle structures and
considerable surgical experience is required for delicate kind of ab-interno surgery8.
Trabeculotomy was developed by Smith in early 1960’s.In the 1970’s and 1980’s
trabeculotomy became an established alternative ab-externo
procedure in surgical treatment of congenital glaucoma9. The aim of the study was to evaluate outcome and
frequency of complications involved in Trabeculotomy.
MATERIAL AND METHODS
A total of 10 children were underwent
trabeculotomy. All patients were registered from Pediatric Ophthalmology
Clinic, Bolan Medical College, Quetta during month of
January and February 2013. The written consent was taken on prescribed form.
Only Primary Congenital Glaucoma patients were registered while secondary
congenital Glaucoma were excluded. Every patient had complete ocular
examination under general anesthesia including anterior segment examination,
measurement of intraocular pressure, corneal diameter, gonioscopy, axial
lengths, fundoscopy, retinoscopy where possible.
Indication
for pressure reducing surgery was
established if 4 of following criteria were fulfilled: (1) typical symptoms (epiphora, photophobia, blepharospasm)
(2) cloudy cornea (3) Increased IOP (4) Increased corneal diameter (5) Increase
in axial length (6) Deep excavated cup (7) PCG in contralateral eye.
Success
criteria was defined as IOP below 15 mm Hg under
general anesthesia, stable axial lengths, disproportional enlargement of
cornea, improvement or at least stability of optic disc excavation (absence of
CDR progression). Visual function was not taken as criteria since mean age of
patients included in study was too young to obtain reliable result concerning
visual acuity.
A Limbal based
conjunctival flap was reflected above. Following peritomy, wet cautry applied.
Subsequently, a 4 x 4 mm lamellar rectangular scleral flap was dissected
crossing the grey white border line zone into clear cornea. Then radial
incision was given in the middle of underlying sclera, approximately 1 mm away
of limbus. The Schlemm’s
canal was located by either scleral cut down via a deep scleral flap or direct unroofing via a deep scleral flap. To confirm about
localization of Schlemm’s canal and avoid false
passage, 6/0 prolene or nylon suture was entered. The
passive entry of suture or prolene in the passage
confirms about proper location of schlemm’s canal.
Then the trabeculotome was gently passed on either
side of incision along the canal for about 5-6 mm, with the other parallel arm
of trabeculotome as a guide and the trabeculotome was rotated in the anterior chamber. The trabeculotome sweeped back and
removed. The same procedure was performed on the other half.
Follow-up period comprised of one, two, four and eight
months respectively.
RESULTS
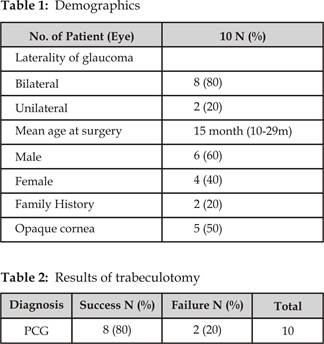
Ten primary operations (Trabeculotomy) were performed. Their
mean age was 15 months (range 10-29m). Among 10 patients, 6 (60%) were male and
4 (40%) were female. 2 (20%) patients have family history of Congenital glaucoma.
Bilateral glaucoma was found in 8 (80%) patients while unilateral glaucoma was
found in 2 (20%). Out of 10, 5 patients had opaque corneas (Table 1). The Trabeculotomy was successful in 8 (80%) patients, while 2
(20%) patients’ needs second surgery (Table 2). Their intraocular pressure was
temporarily controlled with anti-glaucoma medications.
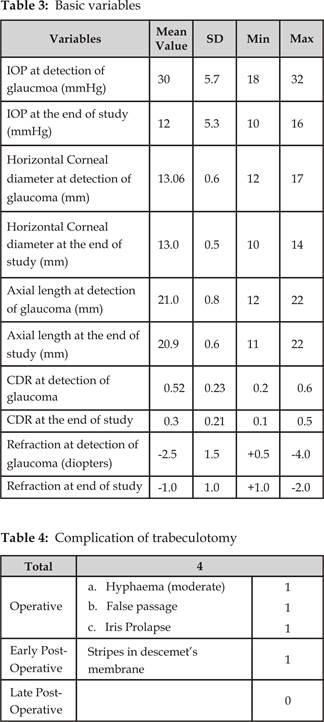
The Intraocular pressure was successfully controlled in 8
(80%) patients. The mean value of Intraocular pressure
was 30 ± 5.7 mm Hg pre operatively and 12 ± 5.3 mm Hg at the end of study
(measured under general anesthesia). Mean horizontal corneal diameter at
detection of glaucoma was 13.06 ± 0.6. The horizontal corneal diameter was
observed as stabilized. Axial length was 21.9 ± 0.8 mm initially. The mean
value of axial length was reduced to 20.9 ± 0.6 mm. The enhancement of CDR was
also stopped. The refraction was possible in 5 patients only (5 patients had
opaque corneas). The myopic shift seems to be stopped finally (Table 3). 4 (40%) patients had
complications comprising of false passage, hyphaema
(moderate), Iris prolapse and stripes in descemet’s
membrane (Table 4).
DISCUSSION
External Trabeculotomy
has proved to be valuable procedure in the surgical treatment of primary
congenital glaucoma. Our results are comparable to those reported by Harms and Dannheim, Singer, Dubois – Poulsen
in their publications.10, 11
One of the
big advantages of trabeculotomy is that it may be
done just as easily in eyes with cloudy cornea as those with clear ones.12
In settings like Balochistan,
where there is lack of awareness, illiteracy, lack of communications the
patients of primary congenital glaucoma presents very late with hazy corneas
and buphthalmos. So this procedure may be beneficial
to treat primary congenital glaucoma in Balochistan,
keeping in view of the advantage of trabeculotomy.
The numbers of patients of congenital glaucoma with opaque corneas are very
high.
Accurate localization of Schlemm’s Canal is the key to successful Trabeculotomy and this is made easier in several ways: If
scleral flap is sufficiently deep and if sclera is dried, one can often see
Iris insertion with portable slit lamp and thus can localize the trabeculum. Use of Prolene (6/0)
or nylon suture: After incising the Trabecular meshwork, there is oozing of
aqueous. Later on 6/0 prolene or nylon suture is
passed to locate the schlemm’s canal. Passive entry
of suture or prolene in the passage is indication of
proper localization of schlemm’s canal.
In this case series, tabeculotomy proved to be successful in 8 (80%) cases and
failed in 2 (20%) cases. Primary congenital glaucoma responds well to surgical
treatment like goniotomy and trabeculotomy
from 80 – 93% as noted by Akimoto at al.13
The failures occur in eyes with
enlarged corneas and in eyes with distorted limbal anatomy like Buphthalmos. 4 patients had complications comprising of
false passage, moderate hyphaema (resolved in one
week), Iris prolapse (relieved by peripheral Iridectomy)
and stripes in Descemet’s membrane.
The Trabeculotomy
provides a significant reduction of IOP i.e. mean IOP was 12 mmHg (measured
under general anesthesia) in most of the patients.14
Lack of Prognostic factor for the
pre-operative IOP should mainly be attributed to measurement in deep
anesthesia. A massive reduction (decrease) of IOP has been shown in animal’s
models after application of halothene. Consequently,
it is important to consider that the normal IOP in infants and children ranges
between 9-12 mm Hg under general anesthesia with halothane.15
In this short term study, we conclude
that at least there is a decrease or stabilization in enhancement of axial
lengths, stability in optic disc excavation. The refraction was possible in 5
patients (5 patients had opaque corneas) indicating low myopia. The progression
of myopic shift was stopped during follow up visits. Although primary
congenital Glaucoma is described as an entity with leading pathological feature
of trabeculodysgenesis resulting in pathologically
increased out flow obstruction.
Prognosis of surgery is thought to be
influenced by the individual nature of dysgenesis.
Axial Length of eye is also a critical factor.
Early manifestation and large ocular
dimensions are key to limited prognosis of any
pressure reducing surgery in PCG.16
As re-surgery is often inevitable in
congenital Glaucoma owing to lifelong expectancy, a step wise surgical strategy
has to be devised, starting with ab interno surgery proceeding to conventional ab externo procedures before
using anti-metabolites or cyclo destructive
procedures.
The present study has several limitations including
relatively small number of patients, short follow-up period, difficulty of
measuring visual acuity in too young, pre-verbal patients and poor patients
compliance.
CONCLUSION
The trabeculotomy may be performed
easily both in cloudy as well as clear corneas. Some of its phases are similar
to Trabeculectomy. The complications are not very frequent. Distorted limbal anatomy Buphthalmic eyes
may affect prognosis of surgery.
Author’s Affiliation
Dr.
Abdul Qayyum
Associate Professor
And Pediatric Ophthalmologist
Department Of Ophthalmology
Bolan Medical College, Quetta
Prof. Dr. Riaz
Ahmed Baloch
Head of department
Department of ophthalmology
Bolan Medical College Quetta
REFERENCES
1.
Chang Ta C,
Cavuoto KM. Surgical management in primary congenital glaucoma: Four
Debates. J Ophthalmol. 2013; 612708.
2.
Morales J, Shahwan SA, Odhayb SA, Jadaan IA, Edward DP. Current surgical options for the management of pediatric glaucoma.
Jr of Ophthalmology.
2013; ID763735: 16.
3.
Khan AO. Genetics of
primary glaucoma. Current Opinion in Ophthalmolgoy.
2011; 22: 347-55.
4.
Mandal A, Chakrabati D. Updates
on congenital glaucoma. Indian J of Ophthalmology. 2011; 59: 148-157.
5.
Kanski JJ,. Cong; Glaucoma in: Kanski
JJ. Editor Clinical Ophthalmology 6th edition, Oxford: Butterworth Heineman, 2009: 245-8.
6.
Taylor D, Hoyt CS. Childhood
Glaucoma in: David Taylor & Creig S Hoyt-editor.
Pediatric ophthalmology and strabismus 3rd edition. Oxford. Elsevier
Saunders. 2005: 460-62.
7.
Mendicino ME, Lynch MG,
Drack A, Beck, Harbin T, Pollard Z, Vela MA, lynn MJ. Long - Term surgical and visual outcomes in primary
congenital glaucoma: 360 degree trabeculotomy versus goniotomy.
Journal of American Association for pediatric ophthalmology & strabismus. 2000;
4: 205-10.
8.
Desilva DJ, KHaw PT, Brooks JL.
Long term outcome of primary congenital glaucoma. J AAPOS. 2011; 15: 148-56.
9.
Moore DB, Oren Tomkins O, Ben-Zion I. Surgical results in management of advanced primary
congenital glaucoma in rural population. Ophthalmology. 2011; 118: 2-3.
10. Harms H, Dannheim R: ’’trabeculotomy-Results
and problems’’ in Mackensen, G: Microsurgery in
Glaucoma, Basel, S. Karger, 1970:
pp.121-131.
11.
Brachet. A, Singer B, dubios-Poulsen A: Complications
de la trabeculotomy. Ann Oculist (Paris), 1972; 205: 1203-1213.
12.
Neely DE. False passage:
A complication of 360 degree suture trabeculotomy. JAAPOS. 2005; 9: 396-7.
13.
Akimoto M. Tanihara H, Negi A, Nagata M. Surgical results of trabeculotomy ab externo for developmental
glaucoma. Arch Ophthalmol 1994; 112: 1540-4.
14.
OuY, Caprioli J.
Surgical management of pediatric glaucoma. Developments in Ophthalmology. 2010;
50: 157-72.
15.
Rodrigues AM, Paranhos A, Montezano FT, De Arruda Melo PA, Prata
J. Comparison between results of
trabeculotomy in primary congenital glaucoma with and without Mitomycin C. Journal of Glaucoma. 2004; 13: 228-32.
16.
Filous A, Brunova B. Results
of modified tabeculotomy in the treatment of primary
congenital glaucoma. JAAPOS. 2002; 6: 182-6.