Cataract
is responsible for over half of blindness worldwide.1 Cataract
surgery is the most commonly performed ocular surgery. Posterior capsule opacification (PCO) is one of the most common late
complications of cataract surgery.2 In one
study the frequency of PCO after cataract surgery was 1.6%, 12.3% and 26.5% at
1, 2 and 3 years respectively.3
PCO
results from migration and proliferation of residual lens epithelial cells in
the capsular bag after cataract surgery, to produce Elschnig’s
pearls or fibroblastic transformation causing capsular fibrosis.4 It
causes gradual deterioration of visual function by obstructing or by scattering
the light rays resulting in decreased visual acuity, decreased contrast
sensitivity, glare or even monocular diplopia.5,6
It also decreases the field of view during therapeutic and diagnostic
procedures.7
The
current treatment of choice for PCO is Neodymium doped: Yttrium-Aluminum-Garnet
(Nd: YAG) laser capsulotomy.
It is relatively safe, gives instantaneous results and can easily be
administered in an out-patient setting.08 The Nd:
YAG laser is solid type of laser, causes disruption of tissues by ionization
mode of action. It has 1064nm wave length, with infrared radiation. It is a
powerful continuous wave laser which is usually Q switched when used to treat
the eye. The 1064nm wavelength is invisible and requires a He-Ne laser red
aiming beam.09
A
number of complications can occur after YAG laser capsulotomy
such as elevation of intraocular pressure, rupture of anterior vitreous face,
damage to intra ocular lens, hyphema, acute iritis, and cystoid macular edema (CMO).10,11
Unusual complications include corneal endothelial damage,12 macular
hole,13 vitreous hemorrhage,10 retinal detachment,08
macular hemorrhage,14 and endophthalmitis.15
Nd: YAG
Laser posterior capsulotomy is a frequently performed
procedure in any ophthalmology department. The purpose of this study was to
find out the complications of Nd: YAG laser capsulotomy in our set up.
MATERIAL AND METHODS
It was
a prospective study conducted over a period of 1 year (from May 2012 to May
2013) at Khyber Eye Foundation Peshawar. A total of 406 patients (437 eyes)
were included in the study.
Inclusion criteria
1.
Patients who had decreased vision due to posterior capsular opacification
2.
More than 6 months duration after cataract surgery with
intraocular lens
3.
Age > 15 years
4. Both genders
Exclusion criteria
1.
Uncooperative patients
2.
Previous history of retinal detachment or vitreoretinal
surgery
3.
Glaucoma
4.
Uveitis
5.
Dislocated IOL
Written
informed consent was taken from all the patients. Before performing YAG laser
detailed history was taken and complete ocular examination was performed
including assessment of visual acuity using Snellen’s
vision chart, slit lamp examination, tonometry with Goldmann
applanation tonmeter and
fundus examination with 90 D/ 78 D lens. Topical anesthetic (0.5% proparacaine hydrochloride) drops were instilled in the conjunctival sac and Abraham’s posterior capsulotomy lens was applied for proper focusing and
stabilization of eyeball. A consultant ophthalmologist performed all Nd: YAG laser capsulotomies using
single shot mode. The amount of energy and number of pulses were adjusted as
required.
Post-laser topical diclofenac (4 times/ day for 1 week) was given to all
patients. Follow up was done at 1 day, 1, 2 and 4 weeks. Detailed eye
examination was performed at each visit including measurement of IOP, anterior
chamber examination, status of IOL, vitreous and fundus examination. Topical
beta blocker therapy was started in eyes with raised IOP.
RESULTS
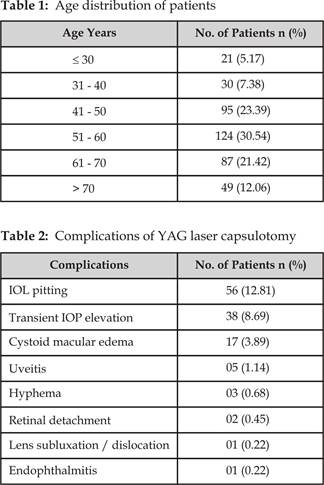
A total
of 406 patients were included in the study including 189 male (46.55%) and 217
female (53.44%). Mean age of the patients was 56.7 years, with a range of 15-82
years. Age distribution of patients is shown in (Table 1). YAG laser capsulotomy was performed in 1 eye in 375 patients and in
both eyes in 31 patients. The number of eyes included in the study was 437.
Mean energy used was 4.1 mJ/ pulse (Range: 1.5 to 8.0 mJ/
pulse). Number of shots varied from 6 to 19 with a mean of 10.7. One or more
complications were noted after YAG laser capsulotomy in
82 eyes (Table 2). Intraocular lens pitting was the most common complication
seen in 56 eyes (12.81%). Transient elevation of intraocular pressure was seen
in 38 eyes (8.69%) and cystoid macular edema was seen in 17 eyes (3.89%).
Serious complications such as retinal detachment (RD) and endophthalmitis
were uncommon and were seen in 2 eyes (0.45%) and 1 eye (0.22%) respectively.
DISCUSSION
YAG
laser capsulotomy is the treatment of choice for
posterior capsular opacification. It is usually a
safe procedure but it may sometime cause complications.08, 10-15
In our
study, IOL pitting was the most common complication seen in 56 eyes (12.81%). In one study IOL damage was seen in 19.2%
cases after YAG laser capsulotomy.08 Khan MY et al found IOL pitting
in 22.4% cases,16 while in another study it
was seen in 3.33% cases.17 Although IOL pitting is one of the common
complications of YAG laser capsulotomy, it is usually
asymptomatic and doesn’t adversely affect the visual functions. In our study, posterior
YAG offset was used to reduce the risk of IOL damage during the procedure,
however the relation of IOL pitting with the extent of posterior YAG offset was
not determined.
The
second most common complication of YAG laser capsulotomy
in our study was transient IOP elevation, which was seen in 38 eyes (8.69%). The
mean IOP elevation was 7.4 mm Hg above the baseline. The frequency of raised
IOP after YAG laser capsulotomy is highly variable,
ranging from 0.8%11 to 82%16 in different studies. However the IOP elevation is usually transient.
In our study, the IOP was well controlled with topical beta blocker therapy (0.5%
levobunolol twice daily) in all cases.
In our study, cystoid macular edema was
seen in 17 eyes (3.89%). In eyes with clinical suspicion, optical coherence
tomography (OCT) was performed to confirm the presence of CMO. In one study CMO was seen in 9.6%.08
In another study CMO was seen in 8.0% cases,20
while in another study it was seen in 0.2% cases.11
Anterior
uveitis was seen in 05 eyes (1.14%) in our study. In one study anterior uveitis
was noted in 46.2% cases after YAG laser.08 In one study conducted
by Muhammad L et al anterior
uveitis was seen in 8.0% cases,18 while in
another study it was seen in 0.6% cases after YAG laser capsulotomy.11
In our study anterior uveitis was very
mild in all cases and responded well to topical steroid therapy.
Hyphema, retinal detachment, lens dislocation /
subluxation, and endophthalmitis were less common
complications seen in our study. These complications were uncommon in other
studies as well.08,11,16-18 Other complications of YAG
laser such as corneal endothelial damage,12 vitreous hemorrhage,10
macular hole,13 and macular
hemorrhage,14 were
not seen in our study.
Most of these complications are
associated with the use of high energy level and poor focusing, although
individual susceptibility also plays an important role. Nevertheless, minimum
energy level combined with minimum number of precisely focused shots for
achieving the desired effect can reduce the risk of complications.11
CONCLUSION
A number of
complications can occur after Nd: YAG laser capsulotomy. The most common of these complications are
intraocular lens pitting, transient intraocular pressure elevation and cystoid
macular edema.
Author’s Affiliation
Dr. Bilal Khan
Vitreo-Retina
Trainee
Lady Reading Hospital
Peshawar
Dr. Mumtaz Alam
Assistant Professor
Ophthalmology Department
Peshawar Medical College
Peshawar
Dr. Mir Ali Shah
Associate Professor
Ophthalmology Department
Lady Reading Hospital
Peshawar
Dr. Bilal Bashir
Vitreo-Retina
Trainee
Lady Reading Hospital
Peshawar
Dr. Asif Iqbal
Vitreo-Retina
Trainee
Hayatabad Medical Complex
Peshawar
Dr. Adnan Alam
Trainee Medical Officer
Lady Reading Hospital
Peshawar
REFERENCES
1.
Polack S, Kuper H, Wadud
Z, Fletcher A, Foster A. Quality of life and
visual impairment from cataract in Satkhira district,
Bangladesh. Br J Ophthalmol. 2008; 92: 1026-30.
2.
Awasthi N, Guo
S, Wagner BJ. Posterior capsular opacification: a problem reduced but not yet eradicated.
Arch Ophthalmol 2009; 127: 555-62.
3.
Erie JC, Hardwig PW, Hodge DO. Effect of intraocular lens design on neodymium:YAG laser capsulotomy
rates. J Cataract Refract Surg. 1998; 24: 1239-42.
4.
McDonnell PJ, Stark W, Green WR.
Posterior capsule opacification:
A specular microscopic study. Ophthalmology 1984; 91: 853-6.
5.
Claesson M, Klaren L, Beckman C, Sjostrand J. Glare and contrast
sensitivity before and after Nd:YAG
laser capsulotomy. Acta Ophthalmol.
1994; 72: 27-32.
6.
Sunderraj P, Villada JR, Joyce PW, Watson A. Glare
testing in pseudophakes with posterior capsule opacification. Eye 1992; 6: 411-3.
7.
Niazi MK, Hanif MK,
Khan HA, Yaqub MA.
Neodymium: YAG; capsulotomy rates following
implantation of PMMA and Arylic Intraocular lenses.
Professional Med J. 2006; 13(4): 538-42.
8.
Burq MA, Taqui AM. Frequency of Retinal Detachment and
Other Complications after Neodymium: Yag
Laser Capsulotomy. J Pak Med Assoc 2008; 58 (10):
550-2.
9.
Elkington AR, Frank HJ, Greaney MJ. Lasers. In: Clinical optics 3rd
Ed. 1999; 216-29.
10.
Shaikh A, Shaikh F, Adwani JM, Shaikh
ZA. Prevalence of different Nd: YAG Laser induced complication in patients with
significant posterior capsule opacification and their
correlation with time duration after standard cataract surgery. Int J Med Med Sci. 2010; 2: 12-7.
11.
Khanzada MA, Jatoi
SM, Narsani AK, Dabir SA, Gul S. Experience of Nd: YAG laser posterior capsulotomy
in 500 cases. J
Liaquat Uni Med Health Sci.
2007; 6: 109-15.
12.
Sherrard ES, Kerr Muir MG. Damage to Corneal
endothelium by Q switched Nd: YAG laser posterior capsulotomy. Trans Ophthalmol Soc
UK. 1985; 104: 524-8.
13.
Wilkins M, Mcpherson R, Fergusson V. Visual recovery under glare conditions following laser capsulotomy. Eye 1996; 10: 117-20.
14.
Majeed A, Bangash T, Muzaffar
W, Durrani O. Macular
Hemorrhage: An Unusual Complication of Nd: YAG Laser Capsulotomy. Pak J Ophthalmol.
1998; 14: 118-20.
15.
Chambless WS. Neodymium: YAG laser posterior capsulotomy
results and complications. J Am Intraocul Implant Soc.
1985; 11: 31-2.
16.
Khan MY, Jan S, Khan MN, Khan S, Kundi
N. Visual
Outcome after Nd-YAG Capsulotomy
in Posterior Capsule Opacification. Pak J Ophthalmol.
2006; 22: 87-91.
17.
Javed EA, Sultan M,
Ahmad Z. Nd:
YAG laser capsulotomy and complications. Professional
Med J 2007; 14: 616-9.
18.
Muhammad L, Jabeen M, Wazir F, Qadir A, Salim M, Ahmad I. Efficacy of Nd:
YAG laser posterior capsulotomy in visual improvement
of patients having posterior capsular opacification. Gomal J Med Sci. 2013; 11:97-100.