Triamcinolone
acetonide is a major therapeutic agent given intravitrealy in various retinal and choroidal
vascular disorders.1-7 The raised
intraocular pressure (IOP) is a major concern of this procedure. The reported
incidence of increase in IOP varies from 27-50% in various studies published in
literature.8-12 Intravitreal triamcinolone
acetonide (IVTA) causes secondary open angle type of
glaucoma. The exact mechanism of rise in IOP is not known but it can be caused
by cortisone crystals blocking the trabecular meshwork or steroid related
decreased phagocytosis of extracellular matrix in meshwork by macrophages. Corticosteroids
are believed to decrease aqueous outflow by inhibiting degradation of
extracellular matrix material in trabecular meshwork, leading to an excessive
amount of debris within the outflow channels with subsequent increase in
outflow resistance.13,14 Steroid induced
glaucoma after IVTA is usually of transient nature but can run a chronic course
in certain patients. Patients having IOP of more than 16 mm Hg, with family
history of glaucoma or having diabetes mellitus are at increased risk of
developing full fledged disease15, 16. An increase in IOP after
IVTA may take up to six months to present12. The rise in IOP can be
variable after IVTA, ranging from 22 mm Hg to more than 40 mmHg, failing to
control with medical therapy and eventually requiring drainage surgery.
We undertook this study to
determine the various treatment options and their effectiveness in controlling
IOP in cohort of patients who received IVTA because of their choroidal and
retinal vascular problems and developed raised IOP > 25 mm Hg.
MATERIAL AND METHODS
This
was a prospective interventional case series conducted at Isra Postgraduate
Institute of Ophthalmology/Al-Ibrahim Eye Hospital, Karachi. Permission to
conduct the research was taken by the ethics committee of the Hospital. The
study design and details of the procedures are described elsewhere12.
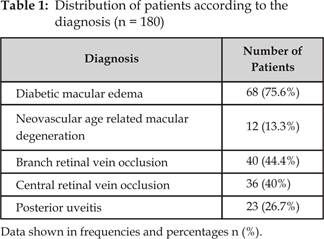
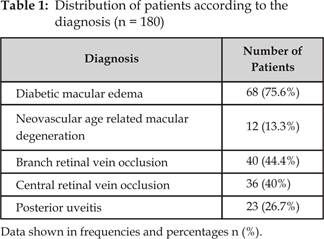
Briefly, 237 eyes of 180 patients received IVTA (4 mg / 0.1 ml) from May 2007
to April 2009 with various choroidal and retinal vascular disorders (Table 1). Patients
having IOP of > 20mm Hg and already receiving anti-glaucoma medication were
excluded from the study.
After
informed consent, a detailed ocular examination was carried out, including best
corrected visual acuity, anterior segment biomicroscopy,
IOP measurement, gonioscopy and fundus examination
using +90 DS lens.
All intravitreal injections were given under sterile conditions
in operating theatre with patients receiving ciprofloxacin 0.3% drops (Ciloxin Alcon, Belgium) one day prior to injection and
continuing for 3 days afterwards. All patients were followed at day 1, 1 week,
1 month, 3 months and 6 months subsequently with mean follow up of one year. At
each follow up visit, patients had charting of vision, IOP measurement and
fundus examination.
A major
aim of this study was to determine the proportion of eyes that had uncontrolled
IOP (> 21 mm Hg) after the injection and the type and effectiveness of the
IOP lowering treatment they received.
The rise in IOP was noticed at
1 week of post injection period but peaked to highest level at 3 months and
continued to show an increase up to 6 months.
Statistical analysis
For data analysis, SPSS (Statistical
Package for Social Sciences) version 17.0 was used. The frequency and
percentages were computed for categorical variables including gender and
diagnosis. For continuous variable IOP, data was shown in mean ± standard
deviation.
RESULTS
Two hundred thirty seven eyes
of 180 patients received IVTA during the study period. The mean age of patients
was 50.86 ± 10.62 years with gender distribution of 99 male and 81 female. Out
of 237 eyes, 117 (49.36%) eyes showed an increase in IOP > 21 mmHg (Fig. 1).
The IOP increased from 13.76 ± 2.79 mmHg to a mean of 15.73 ± 4.5 mm Hg post
injection after 1 week. At 1 month, IOP was increased to 17.3 ± 6.8 mm Hg.
After 3 months, IOP increased to 19.08 ± 8.6 mm Hg and after 6 months IOP was
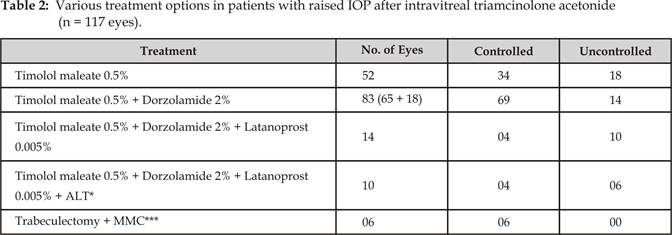
14.38 ± 4.9 mm Hg (p < 0.0001). Fifty two (21.94%) eyes showed an IOP of 21-30
mm Hg. All these eyes were commenced on Timolol maleate 0.5% (Betalol Sante, Pak), one drop
twice a day. Thirty four (14.34%) eyes had controlled IOP < 21 mm Hg, while
18 (7.59%) eyes still had uncontrolled eye pressure.
Sixty five (27.42%) eyes out of
117 eyes had an initial IOP measured > 30 mm Hg. These eyes along with 18
eyes not controlled on single beta blocker therapy (65 + 18 = 83 eyes) were
initiated on combination therapy of Timolol maleate 0.5% + Dorzolamide
2% (Co-dorzal Sante,
Pak). Out of total 85 eyes, 69 (29.11%) eyes responded well on combination
therapy bringing IOP < 21 mm Hg while 14 eyes (5.90%) still had an elevated
IOP of > 25 mm Hg. Four (1.68%) eyes had a further drop in IOP < 21 mm Hg
with addition of Latanoprost 0.005% (Vislat Sante, Pak). Out of
remaining 10 (4.21%) eyes, Argon laser trabeculoplasty
(ALT) was performed, controlling IOP in further 4 (1.68%) eyes. The remaining 6
(2.53%) eyes with uncontrolled IOP of > 25 mm Hg with combination therapy,
prostaglandin analogue and ALT were subjected to trabeculectomy
with adjunctive use of mitomycin-C. All these eyes remained
within range of normal IOP between 10-20 mmHg at mean follow up of one year
(Table 2).
Fig. 1: Raised IOP in total number of eyes following intravitreal
triamcinolone acetonide. Total eyes
237, raised IOP in 117 (49%) eyes.
In essence, out of 117 eyes
showing raised IOP after IVTA, 34 (29.05%) eyes were controlled with single
beta-blocker therapy, 69 (58.97%) eyes were brought into control with
combination therapy. Additional 4 (3.41%) eyes required Prostaglandin analogue
along with combination therapy for IOP control. Another 4 (3.41%) eyes were
controlled with ALT and full medical treatment and remaining 6 (5.12%) eyes
settled down with drainage surgery.
DISCUSSION
Intravitreal
triamcinolone acetonide (IVTA) can be a therapeutically option for the
treatment of various intraocular pathologies including neovascular, oedematous and proliferative disease involving choroid and
retina. It can also be used as an angiostatic agent
in eyes with iris neovascularization, proliferative diabetic retinopathy and
Wet age related macular degeneration. An increase in IOP is a common side
effect with the use of IVTA. The rise in IOP can occur from one week to 6
months post injection. The amount of IOP increase can range from 22-40 mm Hg.
(The raise in IOP can be between 22 and 40 mm Hg) There are certain number of
patients who cannot be controlled on medical therapy and go on to have drainage
surgery. An IOP elevation after IVTA was reported in 40%
of 305 eyes by Jonas and coworkers17. Thirty nine percent of these
eyes were controlled below 21 mm Hg on topical anti-glaucoma medication and
systemic carbonic anhydrase inhibitors with 1% (03) eyes required drainage
surgery. Kocaboraet al8 reported 40 (27%)
eyes out of 147 eyes, showing an increase in IOP of > 25 mm Hg after IVTA.
Thirty three (22.44%) eyes were controlled below 21 mm Hg on combination
treatment of Timolol maleate and Dorzolamide drops,
while 7 (4.7%) eyes required drainage surgery. Park10 and colleagues
reported 26, out of 60 (43.3%) eyes having elevated IOP after 4mg of IVTA.
Intraocular pressure was not controlled despite full anti-glaucoma medication
in 7 (11.7%) eyes. These eyes underwent filtering surgery. In another study
Bashshur18 reported 59 (26.1%) of 226 eyes having IOP higher than 21
mm Hg after IVTA in 4mg dosage. Fifteen eyes (6.63%) had IOP of > 25 mm Hg
treated with combination therapy of Dorzolamide and Timolol maleate, while 3 (1.32%) eyes required surgery.
Compared
to these studies, in our cohort of patients receiving IVTA, 117 out of 237 eyes
showed raised IOP of > 21 mm Hg. Out of these, 34 (29.05%) eyes were
controlled with single beta-blocker, 69 (58.97%) eyes were brought in to
control with combination therapy, while 4 (3.41%) eyes required Prostaglandin
analogue along with combination therapy for IOP control. Another 4 (3.41%) eyes
were controlled with additional ALT and remaining 6 (5.12%) eyes settled down
with drainage surgery.
Severe and intractable IOP
elevation can occur even with full medical treatment after IVTA, with certain
patients necessitating trabeculectomy. This, therefore
requires careful indication of IVTA and long follow up.
CONCLUSION
The benefit of intravitreal
triamcinolone acetonide therapy should be weighed against the risk of increased
IOP, as 50% of our patient receiving IVTA developed raised IOP > 21 mm Hg.
Half of these patients required multiple drugs and almost 5% needed drainage
surgery to control IOP.
Authors Affiliation
Prof. P. S. Mahar
Isra Postgraduate Institute of Ophthalmology
Al-Ibrahim Eye Hospital, Karachi
Dr. A. Sami Memon
Isra Postgraduate Institute of Ophthalmology
Al-Ibrahim Eye Hospital, Karachi
REFERENCES
1.
Karacorlu M, Ozdemir H, Karacorlu S, Alacali N, Mudun B, BurumcekE. Intravitreal triamcinolone as a primary therapy in diabetic
macular oedema. Eye 2004; 19: 382-6.
2.
Hayashi K, Hayashi H. Intravitreal versus retrobulbar
injections of triamcinolone for macular edema associated with branch retina
vein occlusion. Am J Ophthalmol. 2005; 139: 972-82.
3.
Williamson TH, OdonnelA.
Intravitreal triamcinolone
acetonide for cystoid macular edema in nonischemic
central retinal vein occlusion. Am J Ophthalmol.
2005; 139: 860-6.
4.
Park CH, Jaffe GJ, Fekrat
S. Intravitreal
triamcinolone acetonide in eyes with cystoid macular edema associated with
central vein occlusion. Am J Ophthalmol. 2003; 136: 419-25.
5.
Martidis A, Duker JS, Greenberg PB, Rogers AH, Puliafito
CA, Reichel E, BaumalC. Intravitreal Triamcinolone for refractory
diabetic macular edema. Ophthalmology. 2002; 109: 920-927.
6.
Jonas JB, Kreissig
I, Hugger P, Sauder G, Panad-Jonas S, Degenring R. Intravitreal triamcinolone for exudative age related macular
degeneration. Br J Ophthalmol. 2003; 87: 462-8.
7.
Rechtman E, Danis RP, Pratt LM, Harris A. Intravitreal triamcinolone with
photodynamic therapy for subfovealchoroidal
neovascularization in age related macular degeneration. Br J Ophthalmol. 2004; 88: 344-7.
8.
Kocabora MS, Yilmazli C, Taskapili M, Gulkilik G, Durmaz S. Development of ocular hypertension and
persistent glaucoma after intravitreal injection of triamcinolone. Cl Ophthalmol 2008; 2: 167-71.
9.
Jonas JB, Degenring
RF, Kreissig I, Akkoyun I, Kamppler BA. Intraocular pressure elevation after intravitreal triamcinolone
acetonide injection. Ophthalmology. 2005; 112: 593-98.
10.
Park HY, Yi K, Kim HK. Intraocular pressure elevation after
intravitreal triamcinolone acetonide injection. Korean J Ophthalmol.
2005; 19: 122-7.
11.
Jonas JB, Kreissig
I, Degenring R. Intraocular pressure after intravitreal injection of
triamcinolone acetonide. Br J Ophthalmol. 2003; 87:
24-7.
12.
Mahar PS, Memon AS. Frequency and management of raised intraocular pressure following
intravitreal triamcinolone acetonide. JCPSP 2012; 22 (11): 699-702.
13.
Renfro L, Snow JS. Ocular effects of topical and systemic
steroids. DermatolCli. 1992; 10: 505-10.
14.
Wordinger RJ,
Clark AF. Effect of
glucocorticoids on the trabecular meshwork: towards a better understanding of
glaucoma. Prog Retina Eye Res. 1999; 18: 629-67.
15.
Rhee DJ, Peck RE, Belmont J, Martidis A, Liu M, Chang J et al. IOP alterations following intrvitreal triamcinolone acetonide. Br J Ophthalmol. 2006; 90: 999-1003.
16.
Chang YC, Wu W. Elevation of IOP after intravitreal
injection of triamcinolone acetonide in Taiwanese patients. Kaohsiung J Med Sci.
2008; 24: 27-7.
17.
Jonas JB, Degenring
RF, Kreissig I, Akkoyum I, Kamppeter BA. Intraocular pressure elevation after Intravitreal triamcinolone
acetonide injection. Ophthalmology. 2005; 112: 593-8.
18.
Bashshur ZF, Terro AM, El-Haibi
CP, Halawi AM, Schakal A, Noureddin BN. Intravitreal
triamcinolone acetonide: pattern of secondary IOP rise and possible risk
factors. Clin Ophthalmol.
2008; 2: 269-74.