Corneal tattooing has been used not only as a cosmetic treatment
for corneal opacities but for optical reasons as well for centuries. A whitish
corneal scar following keratitis or trauma is cosmetically disfiguring as well
as causes scattering of light and glare. Tattooing such a cornea not only
blends the opacity to the normal eye color which is cosmetically acceptable in
a blind eye but removes the glare in a sighted eye. It has been recommended to
improve the sight of an eye in cases of albinism,
aniridia,
coloboma,
iridodialysis,
keratoconus
or diffused nebulae of the cornea.1,2 In these situations, it
reduces the symptomatic glare associated with a dysfunctional pupil or
scattering of light produced by corneal opacities.
Various methods have been introduced and modified over the years.
Galen (131-210 A.D.)3 is considered to be
the first who dyed human cornea to mask a corneal opacity using reduced copper sulphate. Then Louis Von Wecker4, an oculoplastic surgeon in 1869, used black India ink
to tattoo a leucoma of the eye. He anesthetized the
eye with cocaine and covered the cornea with a thick solution of ink. The
pigment was then inserted into the corneal tissue with a grooved needle
obliquely. In 1901, Nieden5 used an electric tattooing needle based
upon the idea of a fountain pen. Another physician, Armaignac5, used
a small funnel fixed to the cornea by three small points. China ink was filled
into the instrument and injected into the stroma with
a needle. Nowadays, two methods are used predominantly for tattooing the
cornea.
(1) Chemical Method:
this involves using metallic salts which react with each other chemically to
produce a brown-black precipitate that is taken up by the keratocytes
and stain the cornea. The chemicals used are Gold chloride, platinum chloride,
silver nitrate reduced by hydrazine hydrate to a black pigment. The reacting
chemicals are applied over the stroma directly after
peeling the corneal epithelium. This technique was first introduced by Arif O Khan and David Meyer6.
(2) Coloring Method: this technique involves the direct
introduction/impregnation of colored pigments into the corneal stroma. To obtain a
uniform color, the dyeing agent is injected through multiple micro-punctures7
by a needle inserted into the corneal stroma. Various
colored dyes and inks such as Indian ink, organic colors, animal uveal pigment, Chinese ink, soot have been used. To obtain
different shades, surgeons experiment with different combinations of such
chemical products.
The new
advances in technology include using excimer laser to
prepare the corneal bed for tattooing8; lamellar keratectomy offers excellent results in terms of a
homogeneous application of colour9 but for many scars, this is not possible because of irregularity,
thinning, staphyloma or calcification of cornea.
Penetrating keratoplasty (PK) has the risks of
infection and graft rejection and its use for cosmetic purposes is ethically
unacceptable in many parts of the world due to the worldwide shortage of corneal
donors. Mechanized keratopigmentation10 is another costly option.
Alternative methods to improve the aesthetic appearance of disfigured eyes are
cosmetic contact lenses, keratoplasty, wearing ocular
prosthesis with or without an enucleation or evisceration11.
With contact lenses, intolerance frequently develops after prolonged use12
while wearing an ocular prosthesis over a scarred cornea often causes
inflammation, infection and corneal erosion. Hence tattooing of corneal
opacities still has a role for the cosmetic improvement of unsightly corneal
scars. Our study aimed to investigate the potential of corneal tattooing to
improve the ocular cosmetic appearance, to demonstrate its safety, efficacy and
to investigate its potential as an alternative to invasive reconstructive
surgery for the cosmetic correction of disfigured corneas.
MATERIAL AND METHODS
This
prospective, interventional, non-comparative clinical case study was conducted
at the oculoplastic department of Mughal Eye Trust
Hospital, Lahore, a tertiary care referral centre, from June 2012-Dec 2013. 44
consecutive, non randomized patients were included in the study between the age
range of 5 – 60 years (median 21 years). There were 19
females (43.18%) and 25 males (56.82%). All of them were blind in one eye due
to past trauma and desired a cosmetic treatment for their disfigured, white
eye. Ophthalmic examination was performed thoroughly including B scan
ultrasound to exclude intraocular tumor. The depth of corneal opacity, corneal
thickness, the presence and extent of band keratopathy
and corneal vascularization was carefully assessed by biomicroscopy.
Study inclusion criteria was superficial or deep
corneal opacities, band keratopathy, leukokoria (due to a dense cataract with no visual potential
or a pupillary membrane). Patients with phthisical
eyes, thin corneas, corneal edema (bullous keratopathy),
anterior staphyloma and glaucoma were excluded from
the study.
After
fully explaining to the patients and their parents that this procedure was not
meant to restore sight but only their cosmetic appearance and they may need a
repeat procedure, an informed consent was obtained and preoperative photographs
of the patients’ eyes were taken. Corneal tattooing was performed under general
anesthesia in children and local anesthesia (retrobulbar)
in adults. Accurate measurement of corneal area to be tattooed compared to the
second eye was done intra-operatively with a caliper. Corneal epithelium was
debrided using a No.15
Bard Parker-knife. In eyes with band keratopathy (12
cases), first chelation was performed with EDTA solution applied with a cotton
wick on the debrided cornea for 10 minutes. It was then washed off with normal
saline. Any bleeding corneal vessels were cauterized at the limbus.
After drying the cornea with a sponge, 2% Gold Chloride solution was applied
over the corneal stroma and left for two minutes;
then 2% Hydrazine Hydrate solution was applied over the stroma
painted with gold chloride. A black precipitate immediately formed (due to a chemical
reaction between the two solutions) which deeply stained the stroma. It was left in place for 25 seconds and then washed
off with normal saline. Atropine eye drops (1%) and tobramycin eye ointment
were instilled and a pressure dressing was done with a double eye-pad for 24
hour. Postoperatively, all cases were given NSAIDS orally for two days. The
dressing was removed the next morning and Diclofenac
Sodium eye drops were prescribed four times / day, atropine 1% eye drops twice / day and
antibiotic eye drops four times /day for a week. Patients were followed up at
the first, third and fifth post-operative day; then weekly for a period of 1
month and then at 3rd month, 6th month and 1st year post-operatively.
RESULTS
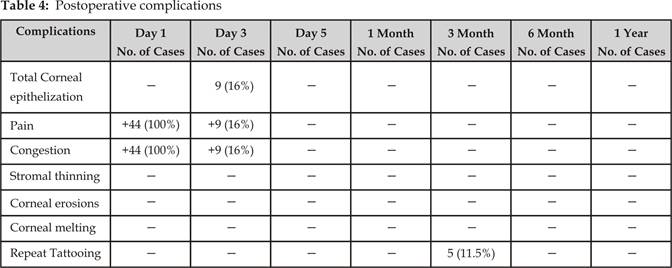
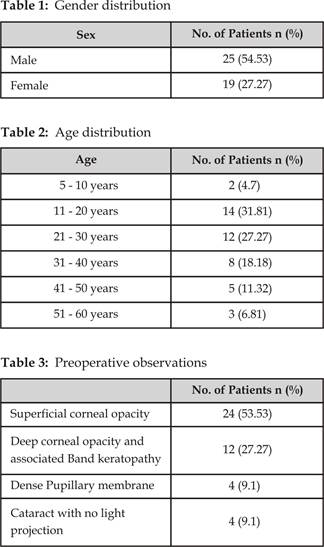
Forty four eyes of 44 patients,
19 females (43.18%) and 25 males (56.82%), (Table 1), with an age range of 5 to
60 years (Table 2) underwent corneal tattooing for disfiguring corneal scars (Table 3). 24 cases
(54.53%) had superficial corneal opacities, 12 cases (27.27%) had deep corneal
opacities with associated band keratopathy. A dense
pupillary membrane with clear cornea was present in 4 cases (9.1%) while a
cataract with no visual potential and an associated corneal opacity was present
in 4 cases (9.1%).
On the first postoperative day
(Table 4), 96% of the patients complained of a moderate foreign body sensation
and exhibited a conjunctival injection which
corresponded to the surgically induced corneal epithelial defect and chemical
reaction. Once the cornea was completely epitheliazed
in 48 hours in 37 cases (84%) and after 5 days in 7 cases (16%), the discomfort
and conjunctival injection resolved. Corneal
infection was not observed in any case. Minimal pigment loss was observed in 5
cases (11.5%) from 3 month onwards and they underwent a repeat procedure.
Corneal melting and corneal erosions were not seen in any case. One year
postoperatively, 42 cases (95.5%) were satisfied with the cosmetic appearance
and were asymptomatic; 2 cases (4.5%) were lost to follow-up.
DISCUSSION
Several
methods for corneal tattooing are in practice today with varying opinions
regarding their safety and success. Chemical tattooing as described in this
study involves a chemical reaction where gold chloride is reduced by hydrazine
hydrate to a black precipitate7. This
metallic precipitate is deposited in the keratocytes
and between the stromal lamellae from which it slowly migrates into the
regenerated epithelium and stays there for a variable time period. It is
important that the bowman's membrane is not damaged during the procedure as its
integrity is very essential for maintaining a strong and healthy epithelial
lining of the cornea. Injury to this membrane either mechanically while
performing epithelial debridement or chemically results in recurrent corneal
erosions which is an intractable and painful condition14. In our
technique, the epithelium was carefully removed under the microscope without
damaging the Bowman's membrane. This gave 95% satisfactory results to our
patients with no corneal erosion seen in any case during follow up.
On the other hand, the method
of direct impregnation of colored dyes
either by a needle or a blade is not 100% safe12. It is very
difficult to determine the exact depth the needle or the blade has traversed
through an opaque cornea and accidental damage to the Bowman's membrane can
easily occur particularly when multiple needle punctures are made. The corneal
epithelium fails to adhere and stabilize at the site where Bowman's membrane is
damaged. Hence the problem of recurrent corneal erosions is frequently seen
because of this technique. Moreover, there is always a risk of accidently
puncturing the cornea at the area of stromal thinning when corneal punctures
are made blindly at multiple sites by a needle. This complication was easily
avoided by our technique.