Original Article
Comparison of Pre and Postoperative
Astigmatism after Cataract Extraction by Phacoemulsification through a 3.2 MM
Clear Corneal Superotemporal Incision
M. Shakaib
Anwar
Pak J Ophthalmol
2014, Vol. 30 No. 3
. . . .
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
. . . . . . . . . . . . . . . . .. . .. . . . . . . . . . . . . . . . . . . . .
. . . . . . . . . . . . . . . .
|
See
end of article for authors
affiliations …..……………………….. Correspondence
to: M. Shakaib Anwar Ophthalmology. Department Rawal Institute of Health Sciences Khana Dak Lehtrar
Road. Islamabad. E mail:
shakaib_2001@yahoo.co.uk …..……………………….. |
Purpose:
To evaluate the difference between pre and postoperative
astigmatism in patients undergoing cataract extraction by phacoemulsification
with intraocular lens implantation through 3.2 mm superotemporal
clear corneal incision. Material
and Methods: A prospective study was performed on 144 eyes of 132 patients.
They were operated upon for cataract between 12/01/2007 and 31/12/2012 by a
single eye surgeon at a private set up. Follow up period was from 6 month to
five years (mean 33 months). The patients included in this study, underwent
cataract surgery by phacoemulsification through 3.2 mm superotemporal
clear corneal incision. Their mean age at the time of surgery was 50.5 years (range: 25 to 76 years). They were divided into two
groups depending upon, “With the Rule” (Group A) or “Against the Rule”(Group B), pre
operative astigmatism. Results:
Before surgery, mean astigmatism in group A patients was -0.83 D
(Diopter) and in those of group B was -0.76 D. After the surgery, mean
astigmatism in group A patients was -1.10 D and in those of group B was -1.10
D. The mean increase in astigmatism post operatively in the two groups was
0.27 D and 0.34 D respectively. Conclusion: Superotemporal clear
corneal incision of 3.2 mm size is favourable in terms of wound stability and
the final optical outcome. When followed up over a long time, the post
operative astigmatism approaches almost the preoperative value although there
may be a negligible increase in it. Key words: Astigmatism, Phacoemulsification, Intraocular
lens. |
Phacoemulsification, and foldable IOLs,
have made cataract surgery through a small incision possible1-3.
Rapid and stable optical recovery is achieved by preventing significant
changes in corneal curvature. The smaller incision size induces less
postoperative astigmatism.1,4,5 The clear
corneal incision technique was introduced by Fine. This has lead to increased
safety, decreased pain, inflammation and surgically induced astigmatism (SIA).6
A positive SIA (horizontal positive cylinder) means “against the
rule” change while a negative SIA (horizontal negative cylinder) signifies a
“with the rule” change.14
Visual outcome after cataract surgery is significantly affected by
the preexisting astigmatism and the one induced by the surgery itself. Usually,
in young people cornea is steepest in its vertical meridian, i.e. AWR
(horizontal negative cylinder). With the advancing age there is a shift to ATR
astigmatism (horizontal positive cylinder). In cataract age group we mostly
find ATR astigmatism.
Modern techniques in cataract surgery aim to achieve optimum
uncorrected visual acuity (UCVA). Different sites and sizes of incisions have
been tried to reduce pre-existing astigmatism which adds to the total post
operative astigmatism. A small incision leads to less astigmatism
postoperatively.2,7-11 Mostly superior or
temporal approaches are preferred by the surgeons. When the preoperative
corneal astigmatism is significant, incision can be placed on the steeper
corneal meridian (parallel to negative cylinder or on the positive cylinder
axis) to reduce overall postoperative astigmatism. Surgically induced astig-matism with small incision surgery is significantly
lower if incision is placed posteriorly nearer to the limbus12. The
size, shape, and place of the incision influence surgically induced
astigmatism. It has an important bearing on the corneal stability13.
A medium sized (3.2 mm) superotemporal
clear corneal incision has the advantage of its size and site. This size does
not allow the wound lips to undergo unnecessary stretching, while injecting the
IOL, avoiding increase and change in axis of the preoperative astigmatism14.
The superotemporal site of the incision in the
oblique meridian, in fact, has a positive effect on both types of astigmatisms
as the steepest meridians are not usually exactly at 180 or 90 degrees15,
rather these lie in between and have a relative vertical or
relative horizontal positions as we have considered in our study.
Generally, a clear corneal incision placed superotemporally
leads to smaller postoperative astigmatism by flattening the horizontal corneal
axis. This has an advantage as ATR astigmatism is common in older age group16.
Another
factor, which can influence the expected out come is
axis in which the IOL haptics are placed. If the IOL haptics are placed at 180°, pre-existing WTR astigmatism
can be reduced and vice versa17. These days
toric intraocular lenses can reduce preexisting
astigmatism quite effectively18. Femtosecond laser assisted cataract
surgery further promises better incision morphology and stability thereby
reducing chances of post operative astigmatism19.
MATERIAL
AND METHODS
A retrospective study was performed on 144 eyes of 132 patients.
They were operated upon for cataract with intraocular lens implantation from 12
Jan 2007 to 31 Dec 2012 with a follow up period of 6 month to five years (mean
33 months). The patients underwent cataract surgery by phacoemulsification
through 3.2 mm superotemporal clear corneal incision
(approx. 0.5mm central to the limbus). At the time of
surgery their mean age was 50.5 years (range: 25 to 76 years). They were
divided into two groups depending upon, “With the Rule” (Group A) or “Against
the Rule” (Group B). In group A, mean astigmatism before surgery was - 0.83 D
while it was -0.76 D in group B.
WTR astigmatism (negative cylinder in the horizontal axis) was considered to be the one in the meridian between 60 and
120 degrees and ATR (negative cylinder in the vertical axis) in the meridian
between 1 and 30 degrees and 150 and 180 degrees. Astigmatism other than
these was classified as oblique.
The patients with oblique or irregular astigmatism were not
included in the study. Similarly the patient who had undergone filtration,
refractive or pterygium excision surgery or had
corneal scaring and opacities, very high or irregular preoperative astigmatism,
were also not included in this study.
Intraocular lens calculations were performed using A-scan
ultrasonography (Quantel Medical 11 M Hz) for axial
length measurements and keratometry using Topcon KR
8800 digital autokerato-refractometer. After
administering peribulbar local anaesthesia with 2% lignocane with 1:200,000 adrenaline, in all the cases a
clear corneal supero-temporal (10-11 clock) incision
(approx 0.50 mm central to the limbus) was made using
a 3.2 mm true cut keratome. A continuous curvilinear capsulorhexis was performed with cystitome.
Phacoemulsifation was performed using system (Ammerican Optics Inc.) machine with 19 Ga
30 degree tip. All patients implanted with single piece, foldable acrylic IOL
with an optical diameter of 6.0 mm (total diameter of 13.0mm), placed in the
capsular bag.
All patients were treated postoperatively with a combination of
dexamethasone 0.1 % and tobramycin 0.3%, three hourly for the first week and
then six and eight hourly over the three subsequent weeks. Topical ofloxacin was given 6 hourly for 1 week postoperatively.
Follow
up for evaluation of astigmatism was performed on Topcon KR 8800 autokerato-refracto-meter from
three months onwards after surgery.
RESULTS
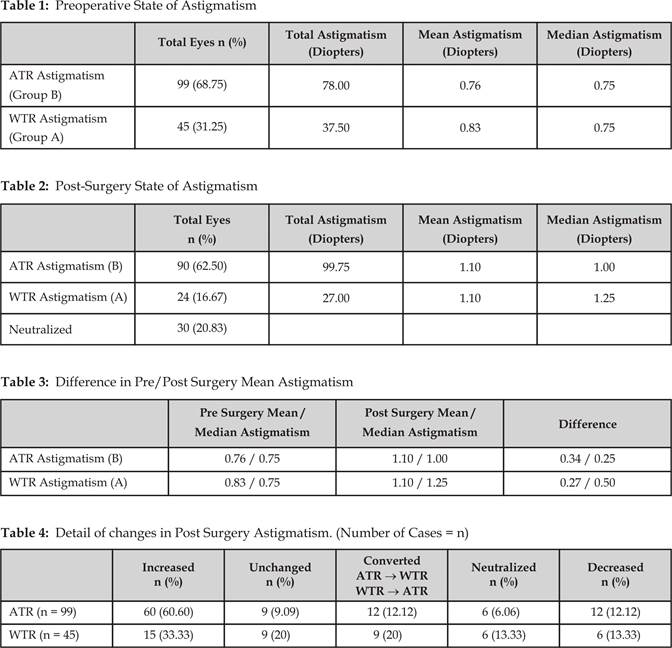
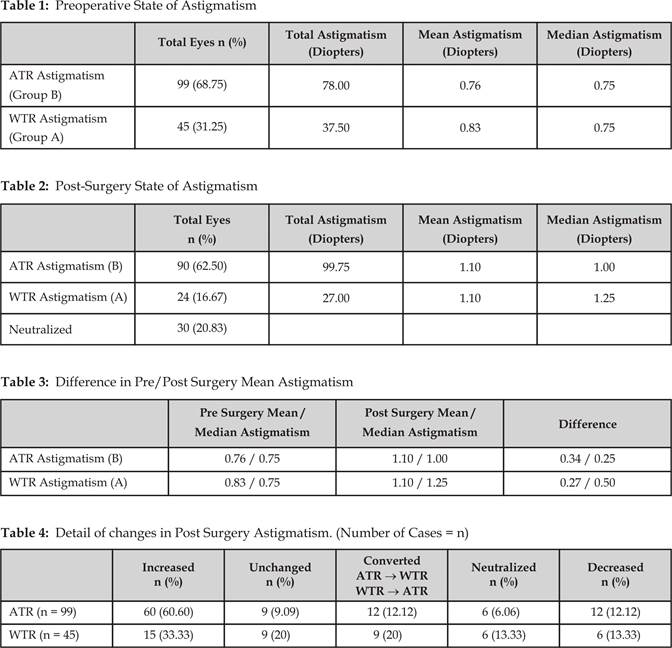
Mean
preoperative astigmatism in group A (45 patients) was - 0.83 and in group B (99
patients) was - 0.76 (Table 1). In group A and and B,
the mean and median postoperative astigmatism were -1.10 and 0.75 diopters
respectively. The mean increase in astigmatism post operatively in the two
groups was 0.27 and 0.34 and the median increase was 0.50 and 0.25 diopters
respectively over 6 months to 5 years follow up (Table 1-3). This showed a
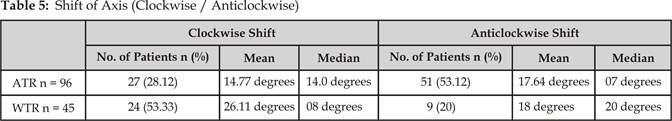
slight shift toward WTR astigmatism post operatively. In group A, 15 (33.33%)
cases showed an increase in astigmatism while 9 (20%) remained unchanged, 9 (20%)
converted to ATR astigmatism, 6 (13.33%) neutralized and 6 (13.33%) experienced
a decrease in WTR astigmatism. In group B, 60 (62.50%) cases showed an increase
in astigmatism while 9 (9.37%) remained unchanged, 12 (12.50%) converted to WTR
astigmatism, 3 (3.12%) neutralized and 12 (12.50%) experienced a decrease in
ATR astigmatism (Table 4). In group A 24 (53.33%) eyes showed a clockwise shift
in the axis (median 11 degrees) and 9 (20%) eyes showed an anti-clockwise shift
(median 20 degrees). In group B 27 (28.12%) eyes showed a clockwise shift in
the axis (median 14 degrees) and 51(53.12%) eyes
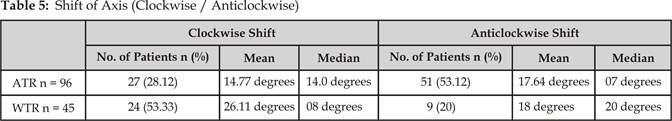
showed an anti-clockwise shift (median 7 degrees)
(Table 5). The rest did not show any shift.
DISCUSSION
In our study we have found that a superotemporal
(10-11 O’ clock) 3.2 mm incision hardly causes any astigmatism or induces any
significant change in the existing preoperative astigmatism, i.e. less than
0.50 diopters generally, when followed over a longer period of time. This correlates
with a similar study carried out by S C Moon et al14.
However the median value showed a slightly more shift on the WTR side (Table
2&3).
Regarding the toric shift, most of the
cases in group A showed a clockwise shift (median 7 degrees) while in group A
the trend was opposite (median shift 8 degrees) in most of the cases (Table 5).
This shift is not very significant during refraction and prescription of
glasses. Less number of cases in both the groups showed wider shift (14-20
degrees). This concluded a minor overall change in the keratometric
readings although the incision was made through the clear cornea.
Our patients showed a slight shift towards higher median WTR
astigmatism with the passage of time. Different studies have demonstrated
flattening of the cornea along the incisional meridian14.
This leads to WTR astigmatic changes with a temporal incision20,21,
comparable with the results of our study.
In a similar study where keratometric
analysis of corneal astigmatism was done after surgery and a comparison was
done between two groups undergoing phacoemulsification through supero-temporal corneal incision and superior scleral
incision. The former did not increase keratometric
corneal astigmatism more than the one by superior scleral incision after three
months of operation22.
The
incision length and location have a bearing on the changes in the horizontal
and vertical meridians of the cornea after cataract surgery. This study was
also affected by these two factors. This fact is also supported by two other
similar studies; small temporal incisions induced less change than superior
incisions14,23.
CONCLUSION
Superotemporal, 3.2
mm clear corneal incision is quite stable and does not significantly increase
post operative astigmatism when followed up over a long (several months to
years) period of time. This size and site of the incision have also proved to
be superior to smaller or larger and superior or scleral incisions
respectively.
One limitation of this study
was that 27 patients did not return for follow up at their designated times.
Author’s Affiliation
Dr. M. Shakaib Anwar
Associate Professor of Ophthalmology
Rawal Institute of Health
Sciences
Khana Dak
Lehtrar Road
Islamabad
E mail: shakaib_2001@yahoo.co.uk
REFERENCES
1.
Leaming DV.
Practice styles and preferences of ASCRS members-1997 survey. J Cataract
Refract Surg. 1998; 24: 552–61.
2.
Drews RC. Five
year study of astigmatic stability after cataract surgery with intraocular lens
implantation: Comparison of wound sizes. J Cataract Refract Surg. 2000;
26:
250–3.
3.
Mamalis
N. Incision width after phacoemulsification with foldable
intraocular lens implantation. J Cataract Refract Surg. 2000; 26:
237–41.
4.
Phleger T, Scholz U, Skorpik C.
Postoperative astigmatism after no-stitch, small incision cataract surgery with
3.5 mm and 4.5 mm incision. J Cataract Refract Surg. 1994; 20:
400–5.
5.
Kohnen T,
Lambert RJ, Koch DD. Incision sizes for foldable intraocular lenses. Ophthalmology.
1997; 104:
1277–86.
6.
Fine IH,
Fichman RA, Grabow HB. Clear corneal
cataract surgery and topical anesthesia. Thorofare,
NJ: Slack; 1993.
7.
Muller-Jensen
K, Barlinn B, Zimmerman H. Astigmatism
reduction: no-stitch 4.0 mm versus sutured 12.0 mm clear corneal incisions. J Cataract
Refract Surg. 1996; 22: 1108–12.
8.
Oshika T, Nagahara K, Yaguchi S. Three
year prospective, randomized evaluation of intraocular lens implantation
through 3.2 and 5.5 mm incisions. J Cataract Refract Surg. 1998;
24:
509–14.
9.
Masket S, Tennen DG. Astigmatic stabilization of
3.0 mm temporal clear corneal cataract incisions. J Cataract Refract Surg. 1996;
22:
1451–5.
10. Kohnen T, Dick B, Jacobi KW.
Comparison of the induced astigmatism after temporal clear corneal tunnel
incisions of different sizes. J Cataract Refract Surg. 1995; 21:
417–24.
11. Rainer G, Menapace
R, Vass C. Surgically induced astigmatism following a 4.0 mm sclerocorneal valve incision. J Cataract Refract Surg. 1997;
23:
358–64.
12.
Ernest
P, Hill W,
Ptvom R. Minimizing surgically induced
astigmatism at the time of cataract surgery using a square posterior limbal incision. J Ophthalmol.
2011; 2011:
243170.
13. Koch PS. Structural analysis of
cataract construction. J
Cataract Refract Surg. 1991; 17: 672–6.
14.
Moon SC, Mohamed
T, Fine IH.
Comparison of surgically induced astigmatisms after clear corneal incisions of
different sizes. Korean
J Ophthalmol. 2007;
21: 1–5.
15.
Lam HY,
Yen KG. Change
in astigmatism after temporal clear corneal cataract extraction in the
pediatric population. Open
Ophthalmol J. 2008;
2: 43–5.
16.
Tejedor J, Murube J. Choosing the location of
corneal incision based on preexisting astigmatism in phacoemulsification. Am J Ophthalmol. 2005; 139: 767–76.
17.
Kim IT,
Park
HYL, Kim
HS. Korean J Ophthalmol.
2011; 25: 22–8.
18.
Miyake T,
Kamiya K, Amano R,
Iida Y,
Tsunehiro S, Shimizu K.
Long-term clinical outcomes of toric
intraocular lens implantation in cataract cases with preexisting astigmatism. J Cataract Refract Surg. 2014 Aug 20. pii:
S0886-3350(14)00942-0.
19.
Mastropasqua L, Toto
L, Mastropasqua A, Vecchiarino
L, Mastropasqua R, Pedrotti
E, Di Nicola M. Femtosecond
laser versus manual clear corneal incision in cataract surgery. J Refract Surg.2014 Jan; 30(1):27-33.
20. Oshika T, Sugita G,
Tanabe T,
Tomidokoro A, Amano S.
Regular and irregular astigmatism after superior versus temporal
scleral incision cataract surgery. Ophthalmology.
2000; 107: 2049-53.
21. Percival P,
Beare N. Clear
cornea sutureless phacoemulsification and astigmatic
decay after two years. Eye (Lond). 1997; 11:
381-4.
22.
He Y, Zhu S, Chen M, Li D..Comparison
of the keratometric corneal astigmatic power after
phacoemulsification: Clear temporal corneal incision versus superior scleral
tunnel incision.
J
Ophthalmol. 2009;
2009:
210621.
23. Merriam
JC, Zheng
L, Urbanowicz
J, Zaider M. Change on the horizontal and
vertical meridians of the cornea after cataract surgery. Trans
Am Ophthalmol Soc. 2001;
99: 187-97.