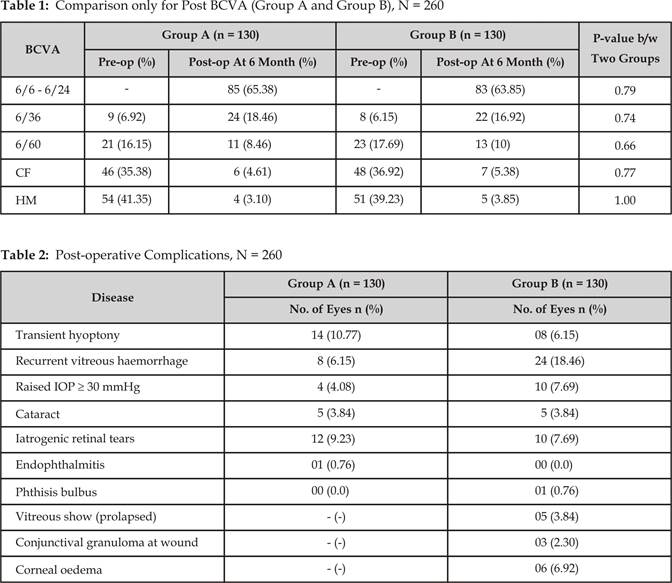
It has
been estimated that 8.5 – 12% population Pakistan suferring
from diabetes mellitus, type-ll is more common and prevalence
of proliferative diabetic retinopathy 2.65 – 5% in our country.1,2 Vitreous haemorrhage due to proliferative diabetic
retinopathy (PDR) is one of major cause of visual impairment and due to
emergence of vitrectomy system and rapid advancement
in surgical techniques for posterior segment pathologies led to improvement in
visual outcome after surgery.
Pars plana vitrectomy (PPV) is one of
the most commonly performed surgical procedure for treatment of various vitreo-retinal diseases. Machemer
et al introduced PPV in 19713. More than Last 30 years, the 3-port
20-gauge PPV remained the standard vitreo-retinal
surgery4. Pars plana vitrectomy involves conjunctival
incision, sclerotomies and suturing but now-a-day’s
20-gauge PPV is also performed transconjunctivally to
make entry wound through the conjunctiva and sclera together, which does not
required conventional suturing. These sutureless self sealing sclerotomies for PPV were first designed by Chen in 19965.
In
2002, Fujil et al introduced the 25-gauge transconjunctival sutureless micro-incision vitrectomy surgery (MIVS).6,7
After few years, in 2005 Eckardt developed the
23-gauge transconjunctival vitrectomy system8.
Though the advances in surgical equipments and techniques,
the vitrectomy procedure requires a skilled and experienced surgeon.
Conventional 3-port 20-gauge PPV need 1.2 mm wide sclerotomies,
performed after conjunctival peritomy
and surgical wound secured with sutures that may cause sub-conjunctival
haemorrhage, congestion and foreign body sensation responsible for
post-operative discomfort as well as prolong surgical time9. In
recent years, the 23-gauge transconjunctival
sutureless vitrectomy (TSV) has become the preferred MIVS system of vitreo-retinal surgeons because of its smaller sclerotomies of 0.72 mm width and leads decrease surgical
trauma, minimum post-operative inflamma-ion, faster
healing and due to its sutureless, shortens the surgical time.10-12
The 23-gauge vitrectomy system has advantage to
overcome the excessive flexibility of instruments used in smaller diameter
25-gauge MIVS, which may cause hindrance in maneuvering the globe during
surgery13.
The
rationale of this study is to compare post-operative visual outcome and
complications between 23–gauge MIVS and 20–gauge pars plana
Vitrectomy.
MATERIAL AND METHODS
In this prospective, randomized clinical trial of 260 patients of
vitreous haemorrhage secondary to proli-ferative
diabetic retinopathy (Fig. 1) were randomly selected for 23 – gauge MIVS (n = 130)
and 20 – gauge PPV (n = 130) for indication of diabetic vitreous haemorrhage
during period of January, 2010 to June, 2012, carried out in LRBT, Free Base
Eye Hospital, Karachi. All surgeries were carried out by one vitreo-retinal surgeon (SZ). The data acquisition was
performed by two investigators (ZI) independently of surgeon, while literature
was reviewed by doctor (WM). The study was conducted under the supervision of
hospital incharge (SFR). The study was approved by
institutional ethical review committee, and informed consent was taken from
each patient.
Cases of diabetic vitreous haemorrhage secondary to type – II
diabetes mellitus, without significant cataract and patients with pseudophakia were included in this study while patients associated
with advanced or complicated PDR like retinal detachment, proliferative vitreo-retinopathy, uveitis, dense cataract and previous
history of vitreo-retinal surgery were excluded from
study and in invisible fundi dynamic B-scan ultrasound carried out to rule out
retinal detachment or any significant fibrotic bands. Pre-operative ocular
& systemic examination of all patients done, including: visual acuity (Snellen’s Chart), ocular adnexa, anterior segment
examination, intra ocular pressure, crystalline lens for opacities (cataract)
and dilated fundal examination with +90 D lens at bio-microscopic slit lamp,
indirect ophthalmoscopy, blood pressure, fasting blood sugar and HbA1c were
checked. All patients were informed about the procedure and written consent
taken. Surgeries were performed by using vitrectomy system) and non-contact
viewing system (EBIOS) for visualization and illumination provided by Xenon
light.
The
rationale of this study is to compare post-operative visual outcome and
complications between 23-gauge MIVS and 20-gauge pars plana
vitrectomy.
Surgical Technique
All
surgeries done under local anaesthesia preferably retrobulbar
with 2 ml of lidocain 2% and 2 ml of bupivacain 0.75% were used. All surgeries were carried out
under strict aseptic measures using povidone iodine
5-10% for periocular paint and conjunctival
fornices with 5% same solution. After applying eye
speculum, self-retaining trocar/cannulae inserted transconjunctivally after 1.5-2 mm displacing conjunctiva
laterally at supero-temporal, supero-nasal
and infero-temporally about 3.5 mm away from the limbus, 300 obliquely to have sclera tunnel in
all phakic patients. The infusion line was connected
to infero-temporal cannula while superior two cannulae for illumination and vitrectomy cutter, after
complete vitreous cleaning, the retina was examined and pan retinal
photocoagulation was done using endolaser (Fig: 2).
Balance salt solution was used as internal tamponade.
At the completion of vitrectomy the superior cannulae were plugged and infusion line was stopped.
Initially superior cannulae were removed with
observing the repositioning of conjunctiva covering the sclerotomies
finally infero-temporal cannula with infusion line
removed and observed repositioning of conjunctiva; finally the sclerotomies in group A, of 23-gauge MIVS left sutureless. (No any patient required suturing in group AIn Group B, 20-gauge sclerotomies
were done with MVR blade and infero-temporally
infusion canula was sutured with vicryl
6/0. At end of surgery, the sclerotomies and
conjunctiva were sutured with vicryl 6/0 (Ethicon,
Johnson and Johnson).
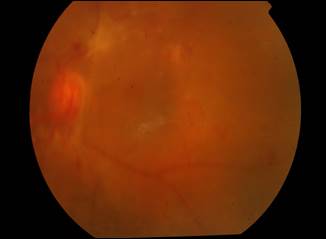
Fig. 1:
Pre operative Fundus photograph of Vitreous Haemorrhage
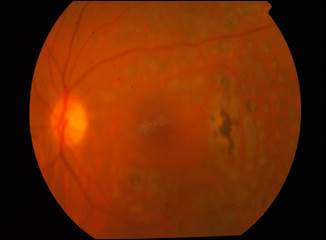
Fig. 2: Fundus photograph after Pars Plana Vitrectomy
with Endolaser
The data was collected for
variables like, age, gender, best corrected visual
acuity (BCVA). Pre-operatively and post-operatively follow up were at day one,
1 week, 1 month, 2 month, 3 month and finally at the end of 6 months visual
acuity measured with Snellen’s chart followed by
refraction (where needed) and various post-operative complications were
evaluated. Variables were statistically analyzed by Wilcoxon test for pre &
post operative BCVA and Chi-square’s Test and Fisher’s Exact Test where applied
for comparison two groups. A P-value
≤ 0.05 considered statistically significant.
RESULTS
Data of
two hundred sixty eyes of 260 patients were analyzed, 130 in each group A for
23-gauge MIVS and group B for 20-gauge PPV. Age range was 30 to 70 years, 73
(56.15%) males and 57 (43.85%) females in group A while 70 (53.85%) males and
60 (46.15%) females in group B. BCVA of two groups were analysed
by applying Wilcoxon test (NPar) to compare pre and
post BCVA of two groups, that showed significant improvement (p-value 0.0001).
BCVA differences in patients of
two groups were insignificant when measured finally at 6 months
post-operatively shown in Table 1. In group A 85 (65.38%) improved between 6/6
- 6/24, 6/36 24 (18.46%), 6/60 11 (8.46%), CF 6 (4.61%), HM 4 (3.10%); whereas
group B improved 83 (63.85%) - 6/6 - 6/24, 22 (16.92%) - 6/36, 13 (10%) - 6/60,
7 (5.38%) - CF, 5 (3.85%) -HM (HM due to ischemic maulopathy
proven by FFA and recurrent vitreous haem:). P-value
of BCVA between two groups remained insignificant. Early visual recovery observed
in group A that might be due to lesser manipulation.
Post-operative complications are summarized the table 2. Only one patient
(0.76%) in group A developed endophthalmitis which
was successfully treated with standard intra-vitreal,
topical and systemic antibiotics and one eye (0.76%) in group B end up into
phthisis bulbus. Inspite of
itrogenic tears, no any patient developed retinal
detachment. Because confluent lasers were applied around
tears.
DISCUSSION
In this
study post operatively BCVA of both groups at 6 months significantly improved
shown in (table 1) from hand movement to between 6/6 to 6/24 in 65.38% (85/130
patients) in 23-gauge group and 63.85% (83/130 patients) in 20-gauge group;
which shows insignificant statistical difference between two groups. A study of
Kim JM et al shows BCVA 6/6 to 6/24 in 72.72% in cases of vitreous haemorrhage
23-
gauge vitrectomy which is much better
improvement than this study14. This difference in visual outcome is
due to variation in case selection. Nataraj AMS mentioned
significant BCVA improvement in his study of 23-gauge and 20-gauge technique
with insignificant statistical difference in two groups, which is comparable to
this study15.