Leukocoria is a
term used for a white pupillary reflex or an altered red reflex on distant
direct ophthalmoscopy,1 and is a grave
cause of visual morbidity in children. The term derives its name from the Greek8
words, ‘leukos’ meaning white, and ‘kore’
meaning pupil. Leukocoria implies opacification of the structures lying within
the visual axis and heralds danger. It is a rare and ominous finding which
signifies serious ocular disease like congenital cataract, retinoblastoma,
advanced retinopathy of prematurity (ROP), persistent hyperplastic primary
vitreous (PHPV), Coat’s disease, uveitis etc, which threaten vision permanently
and some, like retinoblastoma are life threatening.2,3
The
assessment of the red reflex or Bruckner Test by means of the direct
ophthalmoscope is a very simple, useful, quick, non-invasive, and effective
tool for detecting leukocoria in neonates.4
Childhood
blindness varies in etiology according to regional and socioeconomic
differences. Regarding the developing countries; 7 – 31% of childhood blindness
and visual impairment can be avoided, 3 – 28% is preventable, and around 10-58%
can be treated.5 This constitutes a
tremendous public health issue in such countries6. Hence, the need
for screening for potentially blinding ocular diseases arises with enormous
magnitude, to prevent blindness. According to estimates in 2000, 1.4 million
children are blind7 globally, and the majority belongs to developing
countries. In these countries, due to illiteracy, poverty, and unawareness,
there is reluctance to seek medical advice, and often delayed presentation to
the ophthalmologists, with resultant advanced disease or refractory amblyopia,
often with no chance of salvation of vision.
The
importance of neonatal screening for leukocoria is often overlooked and is not
a routine in most maternity or pediatric departments in our country. This
results in delay in diagnosis and seeking of medical treatment, with subsequent
disastrous consequences.
Thus we decided to
undertake a study to routinely screen neonates by distant direct ophthalmoscopy
in order to detect those potentially vision threatening conditions which
present with leukocoria, and manage them promptly. We also embarked to observe
the red reflex variations in different neonates, and whether there existed an
association between the reflex and the various neonatal variables; gestational
age, birth weight, oxygen therapy, phototherapy, and blood transfusion. By this
study, we aim to establish the importance of screening neonates for leukocoria,
which should become a routine practice in all the maternity and pediatric units
of the country. This will result in early detection, prompt referral, treatment
and consequently good visual development of the newborns afflicted with such
disease.
MATERIAL AND METHODS
This descriptive, quantitative
study was carried out by the Department of Ophthalmology with cooperation of
the Department of Pediatrics,

Fig. 1: Distant direct
ophthalmoscopy of a neonate

Fig. 2: Red reflex
assessment
The data was
tabulated and analyzed in the SPSS version 17 Software. Frequencies and
percentages were calculated for the red reflex shades, gestational age, gender,
birth weight, and the neonatal variables (oxygen therapy, phototherapy, and
blood transfusion). The Chi square test was used to analyze any association
between the red reflex and the above variables. The significance level was set
at 95% for each.
RESULTS
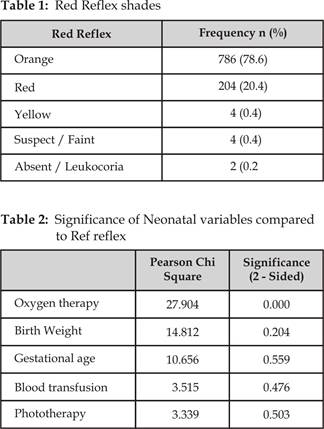
The neonates
examined included 266 males, and 234 females. The red reflex was found to be
normal shades of red or orange in 990 eyes, with orange being predominant in
786 (78.6%), red in 204 (20.4%), yellow in 4 (0.4%), suspect / faint
in 4 (0.4%), and absent / leukocoria in 2 (0.2%) eyes (Table 1). The
yellow, suspect / faint and absent reflexes were examined in detail,
in the Eye Out Patient Department. One of the yellow reflexes had a normal
exam, the other was lost to follow up, one suspect / faint reflex was
found to be bilateral anterior uveitis, with a normal fundus, the other died
before examination, and the neonate with absent reflex had bilateral leukocoria
due to congenital anterior polar and nuclear cataracts, with normal posterior segments.
The child was subsequently operated within 3 weeks and fitted with aphakic
spectacles promptly. The reflexes were symmetrical in hue in 312 (62.4%), and
asymmetrical in 188 (37.6%) neonates. Comparison of the reflex with neonatal
variables resulted in a statistically significant association of the orange hue
with oxygen therapy only (p = 0.000), and no association with gestational age
(p = 0.559), birth weight (p = 0.204), phototherapy (p = 0.503), or blood
transfusion (p = 0.476) (Table 2).
DISCUSSION
Leukocoria is
generally classified1 into pre-lenticular, lenticular, retrolenticular, and mixed presentation leukocoria.
Causes of leukocoria are manifold: the most
devastating being the Retinoblastoma; most commonly presenting with a white
pupillary reflex, with an estimated incidence of 1 in every 15000 – 20000 live
births, and a worldwide mortality of 5 – 11%.9-12 Retinopathy of
prematurity (ROP), previously termed ‘retrolental
fibroplasia’ is one major preventable cause13. Another major cause
is congenital cataract, which represents 10% of the global preventable visual
loss, with an incidence of 1 in every 2000 live births.14-15 Other
causes of leukocoria include Persistent Hyperplastic
Primary Vitreous (PHPV), Coat’s disease, Toxocariasis,
Retinal detachment, Chorioretinal colobomas,
other retinal tumors, corneal scarring, and uveitis to name a few.2,16
The
red reflex seen by illuminating the fundus by means of a direct
ophthalmoscope is caused by light
passing through
the pupil onto the retina, and resultant partial reflecting back of the light
from the retina, through the pupil to give a reddish – brown homogenous reflex
indicating the colour of retina and choroid. The test should be performed with
the ophthalmoscope at 50 cm away, with the dial preferably set at ‘0’, in a
dark room to allow mydriasis and for better contrast. In presence of normal
transparent ocular media the reflex is reddish-orange. Any abnormality or
opacification of the cornea, aqueous humor, lens, vitreous, or retina can
result in a suspect or absent red reflex. Hence, this test is very useful and
any absence of the red reflex, abnormal size, shape, position, non-homogeneity,
presence of dark spots, significant asymmetry, or milky white spots, need
immediate ophthalmologist referral. Variations in colour exist with race due to
difference in fundus pigmentation.17-22
In our
study, we found the red reflex to be of varying shades of red and orange
predominantly, with yellow, suspect or absent reflex in only 5 neonates. We
found bilateral anterior uveitis and congenital cataract in one child each.
Studies carried out on red reflex screening on neonates and children are many
fold.
A study18
carried out in Brazil on 190 neonates found a suspect reflex in 3 newborns.
Five infants were identified with congenital cataract on routine testing, in a
study carried out in
In our
study, a significant association of the red reflex was found, with oxygen
therapy only. Out of the 125 neonates who received oxygen therapy after birth,
predominantly orange reflex was observed in 84 (67.2%) cases, followed by red
in 39 (31.2%) cases. Although, we consider red and orange reflexes to be
normal, larger scale studies are needed to establish a definitive relation of
oxygen therapy if any. We did not include duration of oxygen therapy in our
study. A colour gradient instrument was used in a study carried out in Brazil18
in 2011 to classify the red reflex and significant associations were found
between the instrument and neonatal variables including weight, gestational
age, and oxygen therapy. Here too, orange reflex was predominant in 52.6% of
neonates receiving oxygen; however, no relationship was seen with duration of
exposure. The importance18-28 of red reflex screening of neonates
and children has been established in various countries around the world like
America, Canada, Britain, Israel, and India, to name a few. Studies carried out
by Abramson29 et al and Canzano30 et al recommend
pupillary dilatation for detection of retinoblastoma as a dilated pupil increases
the sensitivity of the red reflex test. We avoided dilating all the patients,
for fear of the known adverse effects of the topical agents, and only dilated
those neonates with very small pupils in which the red reflex was difficult to
discern. This could be a limitation of our study.
The
importance of red reflex testing needs to be realized by ophthalmologists, and
measures to create awareness of this noninvasive and useful test need to be undertaken
in the nurseries and pediatric units of all hospitals, to train their doctors;
with appropriate urgent referral to the ophthalmologist if any abnormality is
detected on routine testing.
The
early detection of such diseases which cause leukocoria would result in saving
vision or lives of children, which would have immense long-term benefits for
those unfortunately afflicted with the disease. Prevention of visual loss is
also our responsibility and we should play our role as much as we can for this
cause. Identification of risk factors such as low birth weight and a positive
family history for certain diseases like Retinoblastoma and congenital cataract
would result in meticulous screening at birth and at frequent follow ups.
Childhood blindness
and visual impairment is a considerable public health issue. Prevention of
visual impairment and blindness in children is an international concern of
foremost priority. Screening for ocular diseases by doctors will play a key
role in early detection, intervention and subsequent management.
CONCLUSION
Screening of
neonates for red reflex assessment with distant direct ophthalmoscopy, for
diagnosing leukocoria is an extremely easy, noninvasive and useful test for
early detection and management of, vision or life threatening diseases, and
needs to become a routine in all hospitals of our country. This will have a
long term effect on the lives of neonates affected by ocular disease.
Author’s Affiliation
Dr.
Sana Nadeem
Assistant
Professor
Department
of Ophthalmology
Jhelum
Road, Rawalpindi
Prof.
B. A. Naeem
Professor
and Head,
Department
of Ophthalmology
Prof.
Parveen Akhtar
Professor
and Head,
Department
of Paediatrics
Jhelum
Road, Rawalpindi
Dr.
Mariam Farooq
Post
Graduate Trainee
Department
of Paediatrics
Jhelum
Road, Rawalpindi
REFERENCES
1.
Tartarella MB, Britez-Colombi GF, Fortes Filho
JB. Proposal of a novel classification of
leucocorias. Clin Ophthalmol. 2012; 6: 991-5.
2.
Patel
N, Salchow DJ, Materin M.
Differentials and approach to leukocoria.
3.
Balmer A, Munier M. Differential
diagnosis of leukocoria and strabismus, first presenting
signs of retinoblastoma. Clin Ophthalmol. 2007; 1: 431-9.
4.
Tuli SY, Giordano BP, Kelly M, Fillipps D, Tuli SS.
Newborn with an absent red reflex. J Pediatr Health Care. 2013; 27: 51-5.
5.
Kong
L, Fry M, Al-Samarraie M, Gilbert C, Steinkuller PG.
An update on progress and the changing epidemiology of causes of childhood
blindness worldwide. J AAPOS. 2012; 16: 507-1.
6.
Maida
JM, Mathers K, Alley CL.
Pediatric ophthalmology in the developing world. Curr Opin Ophthalmol. 2008;
19: 403-8.
7.
World Health
Organization. Preventing blindness in children: report of WHO / IAPB scientific
meeting. Programme for the Prevention of Blindness and Deafness, and
International Agency for Prevention of Blindness. Geneva: WHO, 2000
(WHO/PBL/00.77)
8.
Buscombe C, Headland S.
Infantile Leukocoria: the white pupil. BUJO. 2013; 1: 1-4.
9.
Bukhari S, Aziz-ur-Rehman,
10.
Khurram D, Zaheer N, Hassan S.
Clinical presentation and staging of newly diagnosed intraocular retinoblastoma
according to International Classification of Retinoblastoma. Al-Shifa journal
of Ophthalmology. 2011; 7: 32-8.
11.
Arif M, Iqbal Z, Zia-ul-Islam.
Retinoblastoma in NWFP,
12.
Luo C, Deng YP.
Retinoblastoma: concerning its initiation and treatment. Int J Ophthalmol.
2013; 6: 397-401.
13.
Sabzehei MK, Afjeh SA, Farahani AD,
14.
Rosenfeld SI, Blecher
MH, Bobrow JC,
15.
Simon JW, Buckley EG,
Drack AV,
16.
Haider S, Qureshi W, Ali A.
Leukocoria in children. J Pediatric Ophthalmol Strabismus. 2008; 45: 179-80.
17.
Tamura
MYY, Teixeira LF. Leukocoria and the red reflex test.
Einstein. 2009; 7: 376-82.
18.
Carvalho de Aguiar AS, Ximenes LB, Lúcio IML, Pagliuca LMF, Cardoso
MVLML. Association of the Red Reflex in
Newborns with Neonatal Variables. Rev Latino-Am Enfermagem. 2011; 19: 309-16.
19.
Eventov – Friedman S, Leiba H, Flidel – Rimon O, Juster-Reicher A,
Shinwell ES. The red reflex examination in
neonates: an efficient tool for early diagnosis of congenital ocular disease.
Isr Med Assoc J. 2010; 12: 259-61.
20.
Buckley
EJ, Ellis GS Jr, Glaser S, Granet
D, Kivlin JD, Lueder GT, et
al. Red reflex examination in neonates,
infants, and children. Pediatrics. 2008; 122: 1401-4.
21.
McLaughlin
C, Levin AV. The red reflex. Pediatr
Emerg Care. 2006; 22: 137-40.
22.
Saiju R, Yun S, Yoon PD, Shresta
MK, Shresta UD.
Bruckner red light reflex test in a hospital setting.
23.
24.
Patel
N, Salchow DJ, Materin M.
Differentials and approach to leukocoria.
25.
Li
LH, Li N, Zhao JY, Fei P, Zhang GM, Mao JB, Rychwalski PJ. Findings
of perinatal ocular examination performed on 3573, health full-term newborns.
Br J Ophthalmol. 2013; 97: 588-91.
26.
Muen W, Hindocha M,
Reddy M. The role of education in the
promotion of red reflex assessments. JRSM Short Rep. 2010; 1: 46.
27.
Li
J, Coats DK, Fung D, Smith EO, Paysse E.
The detection of simulated retinoblastoma by using red-reflex testing.
Pediatrics. 2010; 126: e202-7.
28.
Gogate P, Gilbert C, Zin A. Severe visual
impairment and blindness in infants: causes and opportunities for control.
29.
Abramson
DH, Beaverson K, Sangani P,
Vora RA, Lee TC, Hochberg HM, Kirszrot
J, Ranjithan M.
Screening for retinoblastoma: presenting signs as prognosticators of patient
and ocular survival. Pediatrics. 2003; 112: 1248-55.
30.
Canzano JC, Handa JT. Utility for
pupillary dilatation for detecting leukocoria in patients with retinoblastoma.
Pediatrics. 1999; 104: e44.