Among the world’s blind population, 4%
lives in Pakistan; 80% of which is avoidable.1 Cataract is one of
the leading causes of reversible blindness in the world and cataract surgery
consists of major work load of every ophthalmic unit.2
Every procedure whether phacoemulsification,
extracapsular cataract extraction or manual suture less cataract extraction
merits and demerits are being debated by the ophthalmology community but one
consensus remains for every procedure that the postoperative inflammation after surgery should be minimal3.
Anterior chamber inflammation following cataract surgery has been reported up
to 30% varying from mild to severe.4 Post operative anterior chamber
reaction is significant as it may lead increased intraocular pressure (IOP),
corneal edema, endothelial injury, fibrin formation on intraocular lens (IOL) surface, posterior synechia
(PS), posterior capsular opacity (PCO), cystoid macular edema (CME), and
chronic anterior uveitis.
Heparin having anti-inflammatory
properties is being used in pediatric cataract surgery in the form of coatings
on the intraocular lenses 5 and in irrigating solutions to reduce
the post operative inflammation6. We conducted a quasi experimental
study to document the severity of post operative anterior chamber reaction
after adding heparin to the irrigating solution during cataract surgery in
adults.
MATERIAL AND METHODS
This prospective study was conducted in
the Redo Eye hospital, Rawalpindi from Feb
2011 to Dec 2011. Two hundred cases, with ages 50 years to 75 years, were
selected by Convenience (Non Probability) sampling technique for cataract
surgery. They were allotted
a hospital number and had to sign an informed consent for the procedure. Preoperative examinations like slit lamp
examination, intraocular pressure measurement by Goldman's applanation
tonometry, indirect ophthalmoscopy, A-scan and keratometry were carried out for
all cases.
Criteria were
patients diagnosed with senile uncomplicated cataract and pupil diameter equal
or greater than 7 mm after mydriasis.
Exclusion criteria were history of ocular pathology, a
relative afferent pupillary defect glaucoma, uveitis, high myopia, pseudoexfoliation,
or corneal pathology, traumatic, subluxated and posterior polar cataract,
previous ocular surgery, diabetic retinopathy and patients with Fuchs dystrophy
and any ocular surface disease. Dark brown cataracts were also excluded because
of prolonged surgical time. Cases with intra operative complications like
posterior capsular rent were also excluded from the study.
All the cases under went
operation by the single surgeon having expertise in the technique of manual sutureless cataract surgery (MSCS).
At the beginning of the surgery, 1 ml of
heparin sodium (concentration 10 IU/ml) was added to the 500cc balanced salt
solution to irrigate the anterior chamber during the surgery. Procedure was
started with a conjunctival flap made at superotemporal part of the limbus.
Scleral tunnel was constructed using a crescent knife and extended up to 1.0 mm
into clear cornea. A 3.2 mm keratome was used to
access the anterior chamber and the internal corneal incision was extended for
about 0.5 mm more than the external scleral incision. The anterior chamber was
deepened using a standard viscoelastic i.e. 2% hydrooxypropyl
methylcellulose and continuous curvilinear capsu-lorrehexis
of 5 - 6 mm was done using a bent 27 – gauge needle mounted on the irrigating
infusion. The nucleus was delivered by visco expression
and the cortex was washed using a simcoe cannula. A
6.5 mm optic PMMA PC IOL was implanted in the capsular bag inflated by
viscoelastic. The viscoelastic material was replaced by BSS solution .The
integrity of the self-sealing scleral incision was ensured and the cut
conjunctival flap was apposed using a forceps fitted to bipolar diathermy. In the event of any intraoperative complication the
surgical technique was modified accordingly and the case was excluded from the
study.
Standardized postoperative treatment
comprised of prednisolone acetate 1% four hourly and moxifloxacin
four times a day for one week. No oral steroids or topical mydriatic
treatment was given. All patients were followed on the first post operative day
and after one week. At follow up visits, postoperative intraocular cellular
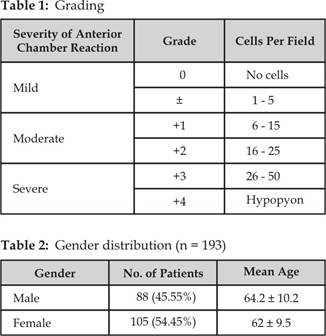
reaction based upon modified Hogan’s classification7, was noted i.e.
cell counting in the anterior
chamber performed by slit-lamp biomicroscopy
examination adjusting the lamp as 3 mm height, 1 mm width and x40 magnification defined as in table 1.
RESULTS
This study was completed in Redo Eye
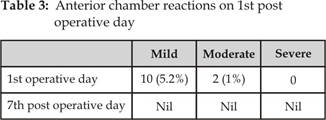
hospital, Rawalpindi in a period of 10 months. A total of 193 cases were
included in the study consisting of 54.45% females and 45.55% males with age
ranging between 50 to 75 years table 2. All patients underwent the same
procedure of MSCS.
On the first post-operative day, 5.2%
patients had mild and 1% cases had moderate anterior chamber reaction (table
3). The patient were put on the standard topical treatment and on first week
follow up the anterior chamber reaction was absent in all of the cases.
DISCUSSION
Age – related cataract is the commonest
cause of avoidable blindness all over the world. Cataract surgery forms the
major workload of eye units worldwide and is a major health care expense. It is
one of the most cost effective of all public health interventions in terms of
restored quality of life. Initially cataract surgery was aimed to prevent
blindness. Now it has progressed to a refractive procedure that aims for post-operative
emmetropia. The quality of vision and early visual
rehabilitation are the important parameters which determine the success of
modern cataract surgery. These two parameters are in turn dependent upon
complications associated with the surgical procedure and the post operative
inflammation.
Addressing the post-operative
inflammation is always a challenge for the ophthalmologist. In the era of
modern phacoemulsification the post operative inflammation is minimal and it is
the procedure of choice in the developed countries. But due to high cost of
phacoemulsification;8 manual sutureless cataract surgery (MSCS) is preferred in the
developing countries.9
During MSCS the iris manipulation is
universal during the some point of surgery10. This may lead to
higher incidence of postoperative iritis. A series
from South India had iritis in 6% and moderate iritis in 3% in the first postoperative week11.
Similarly a study conducted in Pakistan mentioned patients having mild iritis in 16% and moderate iritis
in 5.6% of their cases.12 We added heparin
in the infusion solution and found that there was mild anterior chamber
reaction in 5.2% of our cases. This finding is in accordance to other findings
of the researchers. Xia et al added heparin for cataract surgery and observed
less fibrin and pigment deposits on the lens.13 Similarly
a study conducted in Germany14 concluded that Heparin – sodium added
to the infusion solution during small incision cataract surgery reduced inflammation
in the early postoperative period. A comparative study by Kruger et al15 reported that heparin sodium group had
lesser number of inflammatory cells postoperatively. They also reported a complication of hyphema in their study but
we did not encounter any such complication in our study.
Heparin an anti-coagulant has
associated anti-inflammatory actions16. It inhibits Fibrinous reactions after intraocular surgery by inhibiting
fibroblastic activity17. These unique properties of heparin lead
researchers to use heparin in surface modified IOLs18 and in
pediatric cataract surgery. Similarly Bayramlar and
colleagues19 also concluded that the addition of heparin to the
irrigating solution during surgery decreases postoperative fibrinoid
reaction and late inflammatory complications. The same was concluded by Ihsan Ç and colleagues20 in their study.
We are aware of the short comings of
the study. The sample size was small and it was not a comparative study but to
best of our knowledge we were the first to conduct such a study in Pakistan.
Our results may prove a key role in decreasing the post operative inflammation.
CONCLUSION
We found that by adding heparin in the
irrigating solution there was mild anterior chamber reaction in 5.2% of our
cases and it can reduce the post operative inflammation in adult cataract
surgery.
Author’s
Affiliation
Dr. Yasir Iqbal
Assistant Professor
Department of Ophthalmology
Islamic International Medical
College-Trust
Pakistan Railways Hospital, Rawalpindi
Dr. Sohail Zia
Assistant Professor
Department of Ophthalmology
Islamic International Medical
College-Trust
Pakistan Railways Hospital, Rawalpindi
Dr. Qaim Ali Khan
Assistant Professor
Department of Ophthalmology
Poonch Medical College, Rawalakot, AJK
REFERENCES
1.
Henning A, Kumar J, Yorston
D, Foster A. Sutureless cataract surgery with nucleus extraction: Outcome of a
prospective study in Nepal. Br J Ophthalmol.
2003; 87: 266–70.
2.
Gogate
PM. Small incision cataract
surgery: Complications and mini-review. Indian J Ophthalmol. 2009; 57: 45–9
3.
Gogate PM, Kulkarni SR, Krishnaiah S, Deshpande RD, Joshi
SA, Palimkar A, Deshpande
MD. Safety and efficacy of phacoemulsification
compared with manual small-incision cataract surgery by a randomized controlled
clinical trial: six-week results. Ophthalmology. 2005; 112: 869-74.
4.
Mohammadpour M, Jafarinasab MR, Javadi
MA. Outcomes of
acute postoperative inflammation after cataract surgery. Eur J Ophthalmol.
2007; 17(1):20-8.
5. Çaça I, Şahin A, Cingü AK, Ari S, Alakuş
F, Çinar Y. Effect of low molecular weight heparin (enoxaparin) on
congenital cataract surgery. Int
J Ophthalmol. 2012; 5: 596-9.
6. Kohnen T, Dick B, Hessemer V, Jacobi KW. The anti-inflammatory effect of heparin-containing infusion solutions during phacoemulsification. Ophthalmology. 1995; 92: 297-302.
7.
Hogan MJ, Kimura SJ, Thygeson P. Signs and symptoms of uveitis. 1 Anterior uveitis. Am J Ophthalmol.
1959; 47: 155–70.
8.
Jongsareejit A, Wiriyaluppa C, Kongsap P, Phumipan S.
Cost-effectiveness analysis of manual small incision cataract surgery (MSICS)
and phacoemulsification (PE). J Med Assoc Thai. 2012; 95: 212-20.
9.
Haripriya A, Chang DF, Reena M, Shekhar M. Complication rates of phacoemulsification and manual
small-incision cataract surgery at Aravind Eye
Hospital. J Cataract Refract Surg. 2012; 38: 1360-9.
10. Parikshit MG. Small incision cataract surgery: Complications and mini-review. Indian J Ophthalmol. 2009; 57: 45–9.
11. Srikant KS, Sujata D, Suryasnath R. Blumenthal technique and its modification: The glory of anterior chamber maintainer. Indian J Ophthalmol. 2010; 58: 86.
12.
Zaman M, Qadir A, Maooz,
Shah I, Rehman I, Farooq T. Cataract a nigra
(black cataract): a challenging task made easy with sutureless manual
extracapsular cataract extraction. J ayub med coll abbottabad. 2011; 23:
108-10.
13.
Xia XP, Lu DY, Wang LT. A clinical study of inhibition of secondary cataract with
heparin. J Chung Hua
Yen Ko Tsa
Chih. 1994; 30: 405-7.
14.
Kohnen T, Hessemer V, Koch DD, Jacobi
KW.
Effect of heparin in irrigating solution on inflammation following small
incision cataract surgery. J Cataract Refract Surg. 1998; 24: 237-43.
15.
Kruger A, Amon M, Formanek
CA, Schild G, Kolodjaschna
J, Schauersberger J. Effect of heparin in the irrigation solution on postoperative
inflammation and cellular reaction on the intraocular lens surface. J Cataract Refract Surg. 2002; 28:
87–92.
16.
Dada T. Intracameral
heparin in pediatric cataract surgery. J Cataract Refract Surg. 2003; 29: 1056.
17.
Wilson ME, Trivedi
RH. Low molecular-weight heparin in the intraocular irrigating
solution in pediatric cataract and intraocular lens surgery. Am J Opthalmol.
2006; 141: 537–8.
18.
Koraszewska-Matuszewska B, Samochowiec-Donocik E, Pieczara
E, Flilipek E. Heparin-surface-modified PMMA intraocular lenses in children in
early and late follow up. Klin
Oczna. 2003; 105: 273-6.
19. Bayramlar H, Totan Y, Borazan M. Heparin in the intraocular irrigating
solution in pediatric cataract surgery. J Cataract Refract Surg. 2004; 30: 2163–9.
20. Ihsan Ç, Alparslan
Ş, Abdullah KC, Şeyhmus A, Fuat A, Yasin Ç. Effect of low molecular weight heparin (enoxaparin) on congenital
cataract surgery. Int
J Ophthalmol. 2012; 5: 596–9.