Metabolic syndrome (MS) is a common
condition occurring in diabetic patients and is characterized by the presence
of glucose intolerance, hypertension, central obesity, low high density lipoproteins
(HDL) and high triglycerides. Over-secretion of insulin with peripheral
resistance to insulin action is believed to underlie this syndrome. The
micro-vascular changes associated with MS include diabetic retinopathy,
nephropathy and neuropathy.1,2,3
Metabolic
syndrome (MD) is not an uncommon condition in diabetic patients and
approximately 70-80% of diabetics develop metabolic syndrome (MS) in their
life.2 In Indian population the prevalence of MS is 73.3% in
comparison to the Indian immigrants in USA who have 77% prevalence.4 In
Japanese and Western population the prevalence of MS is reported to be 58.5%
and 77.6% respectively.5,6 The prevalence
is higher in women (83.3%), compared to men (65.3%). Diabetic retinopathy is an
important feature of metabolic syndrome in patients with diabetes with a
prevalence of 16.9%.2
The correlation
between the micro-vascular complications of diabetes and metabolic syndrome
including diabetic retinopathy are well documented.5,7
However not enough literature and data is available in Asian population.
It has been
found that in metabolic syndrome (MS) the risk factors for retinopathy is
elevated HBA1C level, and duration of diabetes, while nephropathy
include hypertension and increased body mass index as risk factors in addition
to elevated HBA1C level, and duration of diabetes.2 In a
study from Faisalabad, the frequency of retinopathy among patients with
diabetes mellitus and metabolic syndrome was found to be 41.4%8,
while in another study from Lahore it was 25%.9
The rationale of
our study is to find out the prevalence of Diabetic Retinopathy in our local
population with type 2 diabetes mellitus having metabolic syndrome. Although
local studies are available in literature but most of them are either
comparative in nature or having controversial results as mentioned above
(studies from Lahore and Faisalabad).
We also tried to generate local
statistics about the magnitude of the retinopathy among diabetic people living
with metabolic syndrome. The results of this study will be compared with
already available local and international literature and if found to be
significantly high, will be shared with local health professionals to device
future recommendations for the prevention and control of the problem. Also this
study will provide us frequency of different grades of retinopathy which has
not been studied locally and will provide us with current statistics about the
most common grade of retinopathy among patients with type II diabetes and
metabolic syndrome.
MATERIAL
AND METHODS
The study was
conducted in Medical Department, Post Graduate Medical Institute, Lady Reading
Hospital Peshawar from March
2011-August 2011. It was a Descriptive Cross Sectional Study, and sampling
technique used was Consecutive Non-probability sampling. A written permission
from the hospital ethical committee was obtained. All patients presenting to
the Medical outpatient department (OPD) of LRH with diabetes of minimum five
years duration were worked up thoroughly for metabolic syndrome by clinical
examination & investigations. Those patients found to have metabolic
syndrome were included in the study and were dealt with on OPD basis or
admitted to the Medical ward where routine investigations as full blood count,
urea, blood sugar, electrolytes, ECG and Echocardiography were done. Already diagnosed cases of retinopathy
like; vasculitis, rheumatoid, systemic lupus erythematosis, radiation retinopathy, and systemic disease that will affect visual acuity
evaluation (for example: CVA), Opaque cornea and vitreous were excluded from
the study.
A written
informed consent was obtained from all the patients. Fundoscopy
of all patients was performed either on OPD basis or after the admission to
detect retinopathy and its different grades. All the fundoscopies
were performed by senior ophthalmologist having got minimum of 5 years
experience in ophthalmology. All the information is recorded on preformed
proforma. An exclusion criterion was followed strictly to control confounding
variables and bias in the study result.
The data was analyzed in SPSS for
windows version 10.0. Continuous variables like age and duration of diabetes
were presented as Mean + Standard deviation. Qualitative variables like
gender, retinopathy and its grades are presented as frequency and percentages. Retinopathy was stratified among age,
gender and duration of diabetes to see the effect modifications. All the
results are presented as tables and graphs.
RESULTS
The study comprised a total of 201
patients of type II diabetes mellitus, having minimum 5 years duration of
diabetes.
The mean age of diabetic patients were 39 ± 12.2 years. The
minimum age in our study was 30 years and maximum age was 70 years.
Distributing the sample in different age groups, we found that 35 (17.4%) were
in the age group 30-39 years, 70 (34.8%) were in the age group 40-49 years, 70
(34.8%) were in the age group 50-59 years while 26 (12.9%) were in the age
group 60+ years.
Considering the
duration of diabetes condition among subjects recruited, in this study, participants
were grouped into: > 510 years with 61 (30.3%) of the sample, 11-15 years
with 75 (37.3%) of the sample while in the group with duration of diabetes of
15+ years we had 65 (32.3%) of the overall sample of 201.
While distributing the sample with regards to gender, we
found that male gender contributed 91 (45.3%) of the sample and female gender
contributed
110 (54.7%) of the overall sample.
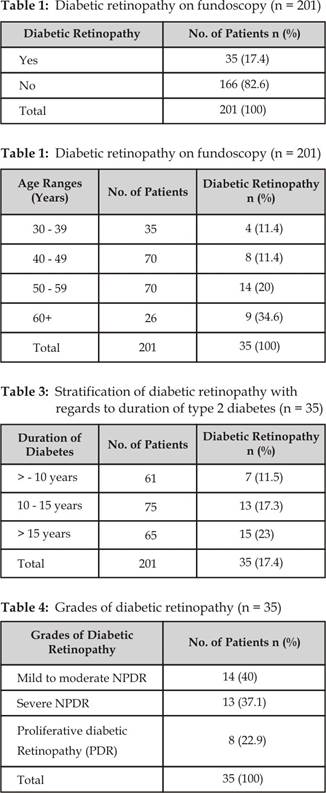
On fundoscopic examination of all the diabetic individuals included
in the study, Diabetic Retinopathy (DR) was observed in 35 (17.4%) of the
patients (Table 1). While looking into the gender wise stratification of the
DR, we found that out of total 91 males, 13 (14.3%) had DR and out of total 110
females, 22 (20%) had DR. Stratifying the DR with regards to age groups, we
found that most of the DR were observed in older age groups, out of 35 in the age group 30-39 years 4
(11.4%) had DR, out of 70 in the age group 40-49 years 8 (11.4%) had DR, out of
70 in the age group 50-59 years 14 (20%) had DR and out of 26 in the age group
60+ years 9 (34.6%) had DR (Table 2).
While stratifying the diabetic retinopathy with regards to
duration of diabetes, we found that most patients of diabetes were in the
prolonged duration of diabetes suggesting that as the diseases progresses, the
chances of developing diabetic retinopathy becomes higher. Out of 61 patients
in the group >510 years with 7 (11.5%) had DR, in the group with duration of diabetes
11-15 years out of 75, 13 (17.3%) had DR while in the group with duration of
diabetes of 15+ years out of 65 patients, 15 (23%) had DR (Table 3).
The grades of retinopathy are also studied in this research project and
it was seen that out of total 35 patients with diabetic retinopathy, 14 (40%)
were in the mild to moderate non proliferative diabetic retinopathy (NPDR)
group, 13 (37.1%) were in the severe non proliferative diabetic retinopathy
(NPDR) group and remaining 8 (22.9) were in the proliferative diabetic
retinopathy (PDR) group (Table 4).
DISCUSSION
Metabolic syndrome (MS) is a specific
disease entity as reported by National Cholesterol Education Programs ATP III
report. Patients with this syndrome shows increased incidence of micro-vascular
diseases.10 Many
studies showed association between hypertension, diabetes, cardiovascular
diseases and micro-vascular retinal disease.11-16 In
our study we addressed the frequency of diabetic retinopathy in diabetic
patients with metabolic syndrome.
The study conducted by Fisbee JC
showed experimentally in rats having obesity, diabetes and metabolic syndrome
that they have narrow skeletal muscle arterioles and impaired arteriolar
reactivity to vaso-active stimuli.17 While study conducted by Irnving
RJ and Serne EH et al14-16 showed changes
in the structure and function of microcirculation in skin and skeletal muscles
in patients with metabolic syndrome.
After 20 years,
nearly 60% people with type-1 diabetes and around 40% with type-2 diabetes have
proliferative diabetic retinopathy. In diabetic patients there is venular dilatation resulting in hyperperfusion
which inturn causes hypoxia and lactic acidosis.18,
19 This venular dilatation is related to the
duration of diabetes, raised HbA1C level and high body mass index as
shown by Winconsin Epidediologic
Study.20, 21 On the basis of all these facts, diabetic retinopathy
can be explained in metabolic syndrome (MS) as a consequence of micro-vascular
changes associated with inflammation and endothelial dysfunction resulting in
decrease perfusion and hypoxia.
Our study showed
relationship between metabolic syndrome (MS) and diabetic retinopathy. In our
study, the prevalence of diabetic retinopathy among diabetics with metabolic
syndrome was 17.4% which is lower than that (21-60 %) reported in other studies
conducted in Karachi and other cities in Pakistan.22 The reason behind these differences could be that most of
those studies were done on inadequate sample size while our study took 201
patients. It may have caused an overrepresentation of diabetics in the sample
because several eye diseases are more prevalent among diabetics than their
non-diabetic counterparts. Second, a third of diabetics did not participate in
the screening for diabetic retinopathy which may have either overestimated or
underestimated the prevalence of diabetic retinopathy, depending on the rates
of diabetic retinopathy among non-respondents.
In our study,
women had a slightingly greater prevalence of diabetic retinopathy than men
(20% vs. 14.3%). The most prevalent type of diabetic retinopathy is our study
was mild to moderate non proliferative diabetic retinopathy (NPDR) which
accounted for 40% of the cases. In a study by Khan in Karachi,22 background diabetic retinopathy
accounted for 79.1% of the cases compared with 92%, 89.3-94.0% and 69.8% in
studies conducted in Australia, India and Oman, respectively. Severe
proliferative diabetic retinopathy (NPDR) was not so far in the race and the
reported frequency in our study was 37.1%. This is lower than those reported in
hospital based studies in Pakistan and elsewhere. The severity of retinopathy
is primarily related to the duration of diabetes, and exposure to various
internal and external ocular factors. This lower prevalence of proliferative DR
can be explained by the fact that majority of our participants were young. Many
studies have found duration of diabetes to be an important predictor of
diabetic retinopathy.23, 24
The strength of
our study includes large sample size (201) and the objective documentation of
signs by both ophthalmologists and physicians. However considering the limitations
of our study it is important to mention that our study was cross-sectional and
prospective data are needed to document the relationship between the
micro-vascular changes including diabetic retinopathy and metabolic syndrome.
To conclude our study, we documented
cross-sectional association between diabetic retinopathy and metabolic syndrome
(MS) in diabetic patients. We recommend further prospective studies to clearly
establish association between metabolic syndrome (MS) and micro-vascular
abnormalities in diabetic patients.
CONCLUSION
Diabetic retinopathy is the commonest cause of visual
impairment in diabetic patients with metabolic syndrome with non-proliferative
diabetic retinopathy more common than proliferative diabetic retinopathy. It
necessitates regular follow up of these patients to prevent development of
proliferative disease and its complications. More studies are recommended
before making recommendations for modifications in principles of its
management.
Authors Affiliation
Dr. Mohammad Asghar
Medical Officer
Medical A unit
Lady Reading Hospital, Peshawar
Dr. Mubashir Rehman
Medical Officer
Department of Ophthalmology
Lady Reading Hospital, Peshawar
Dr. Mohammad Zahid Khan
Medical Officer
Department of Endocrinology
Lady Reading Hospital, Peshawar
Dr. Muhammad Abdur Rehman
Assistant Professor
Medical A unit
Lady Reading Hospital, Peshawar
Dr. Mohammad Zeeshan Tahir
Medical Officer
Department of Ophthalmology
Lady Reading Hospital, Peshawar
REFERENCES
1.
Muhammad A, Gamal
N, Fawaz N. Increased
Prevalence of Micro vascular Complications in Type 2 Diabetes Patients with the
Metabolic Syndrome IMAJ. 2006; 8: 37882.
2.
Raman R,
Gupta A, Pal SS, Ganesan S, Venkatesh
K, Kulothungan V, Sharma T. Prevalence
of Metabolic Syndrome and its influence on micro vascular complications in the
Indian population with Type 2 Diabetes Mellitus. (SN-DREAMS, report 14) Diabetology &
Metabolic Syndrome. 2010; 2: 6-7.
3.
Szalat A, Raz I. Metabolic syndrome and microangiopathy. Ist
Med Assoc J. 2006; 8: 424.
4.
Foucan L, Deloumeaux J, Donnet JP, Bangou J, Larifla L, Messerchmitt C, Salmi LR, Kangambega P: Metabolic syndrome components in
Indian migrants with type 2 diabetes. A matched comparative study. Diabetes Metab. 2006; 32: 337-42.
5.
Bonadonna RC, Cucinotta D, Fedele D, Riccardi
G, Tiengo A: The metabolic syndrome is a risk
indicator of microvascular and macrovascular
complications in diabetes: results from Metascreen, a
multicenter diabetes clinic-based survey. Diabetes care. 2006; 29: 2701-7.
6.
Iwasaki T, Togashi
Y, Ohshige K, Yoneda M,
Fujita K, Nakajima A, Terauchi Y: Neither the presence of metabolic
syndrome as defined by the IDF guideline nor an increased waist circumference
increased the risk of microvascular or macrovascular complications in Japanese patients with type
2 diabetes. Diabetes Res Clin Pract.
2008; 79: 427-32.
7.
Kilpatrick ES, Rigby AS, Atkin SL: Insulin resistance, the metabolic
syndrome, and complication risk in type 2 diabetes: double diabetes in the
Diabetes Control and Complications Trial. Diabetes care. 2007; 30: 707-12.
8.
Hassan M, Akhtar
M, Akhtar N. Prevalence of Retinopathy and Its
Associated Factors in Type-2 Diabetes Mellitus Patients Visiting Hospitals and
Diabetic Clinics in Faisalabad, Pakistan. Pakistan J. Zool. 2010; 42: 41-6.
9.
Ghani U, Niaz Z, Cheema
TM, Abaidullah S, Salman S, Latif
F. Determining
the Association Between retinopathy and metabolic syndrome in Patients with
Type 2 Diabetes Mellitus Visiting Mayo Hospital, Lahore. ANNALS. 2010; 16:
101-4.
10.
Executive Summary of The Third
Report of The National Cholesterol Education Program (NCEP) Expert Panel on
Detection, Evaluation, And Treatment of High Blood Cholesterol In Adults (Adult
Treatment Panel III). JAMA. 2001; 285: 248697.
11.
Klein R, Sharrett
AR, Klein BE, Chambless LE, Cooper LS, Hubbard LD, Evans G . Are retinal arteriolar abnormalities
related to atherosclerosis? The Atherosclerosis Risk in Communities Study. Arterioscler Thromb Vasc Biol. 2000; 20: 1644-50.
12.
Wong TY, Klein R, Sharrett
AR, Schmidt MI, Pankow JS, Couper DJ, Klein BE, Hubbard LD, Duncan BB . Retinal arteriolar narrowing and risk
of diabetes in middle-aged persons. JAMA. 2002; 287: 252833.
13.
Wong TY, Klein R, Sharrett
AR, Duncan BB, Couper DJ, Klein BE, Hubbard LD, Nieto FJ. Retinal arteriolar diameters and risk
of hypertension. Ann Intern Med. 2004; 140: 24855.
14.
Irving RJ, Walker BR, Noon JP, Watt GC,
Webb DJ, Shore AC. Microvascular correlates of blood pressure, plasma
glucose, and insulin resistance in health. Cardiovasc
Res. 2002; 53: 2716.
15.
Serne EH, Ijzerman RG, de Jongh RT, Stehouwer CD. Blood pressure and insulin resistance:
role for microvascular function?.
Cardiovasc Res. 2002; 55: 4189.
16. Serne EH, Stehouwer CD, ter Maaten JC, ter Wee PM, Rauwerda JA, Donker AJ, Gans RO. Microvascular
function relates to insulin sensitivity and blood pressure in normal subjects.
Circulation. 1999; 99: 896902.
17.
Frisbee JC. Remodeling of the skeletal muscle
microcirculation increases resistance to perfusion in obese zucker
rats. Am J Physiol. 2003; 285: 10411.
18.
Skovborg F, Nielsen AV, Lauritzen E, Hartkopp O. Diameters of the retinal vessels in diabetic and normal
subjects. Diabetes. 1969; 18: 2928.
19.
Grunwald JE, DuPont J, Riva CE. Retinal haemodynamics
in patients with early diabetes mellitus. Br J Ophthalmol.
1996; 80: 32731.
20.
Klein R, Klein BEK, Moss S, Wong TY,
Hubbard LD, Cruickshanks KJ. Retinal vascular abnormalities in
persons with Type 1 diabetes. The Wisconsin Epidemiological Study of Diabetic
Retinopathy. Ophthalmology. 2003; 110: 211825.
21.
Wong TY, Shankar A, Klein R, Klein BE. Retinal vessel diameters and the
incidence of gross proteinuria and renal insufficiency in people with type 1
diabetes. Diabetes. 2004; 53: 17984.
22.
Khan MNA, Khan FA, Sultana S, Dilawar M, Ijaz A, Khan MJA, et
al.
Impact of new diagnostic criteria of diabetes mellitus. J Coll
Physicians Surg Pak 2007; 17:32730.
23.
Massin PA, Erginay B, Haouchine AB, Mehidi M. Retinal thickness in healthy and diabetic
subjects measured using optical coherence tomography mapping software. Eur J Ophthalmol. 2008; 12:
102-12.
24.
Yamamoto TN, Akabane
S.
Vitrectomy for diabetic macular edema: the role of posterior vitreous
detachment and epimacular membrane. Am J Ophthalmol. 2007; 132: 69-97.